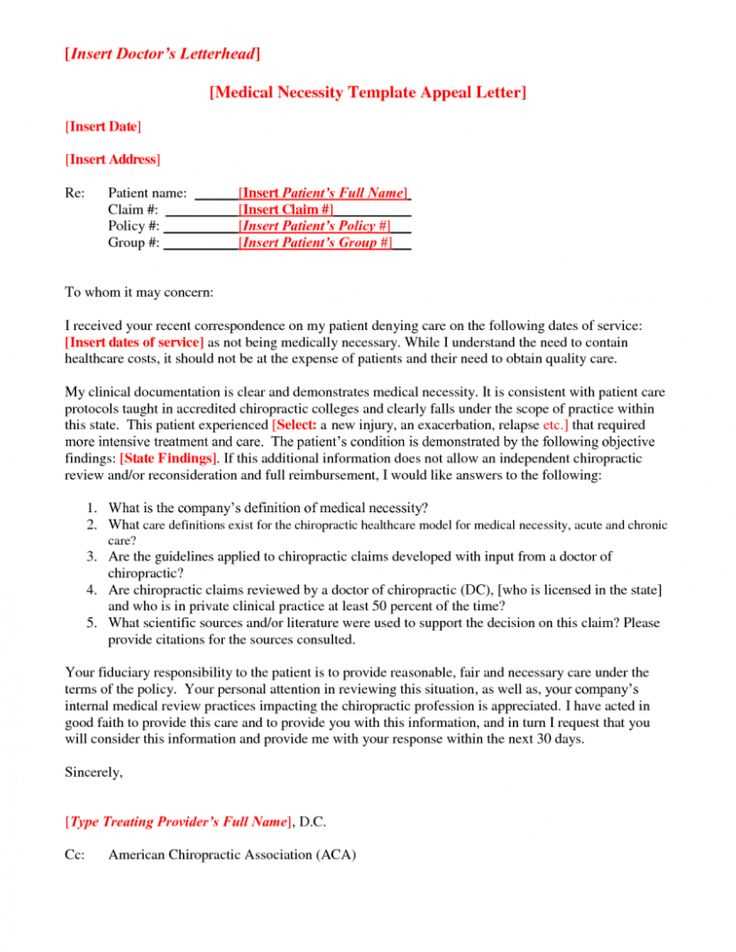
Letter medical necessity template
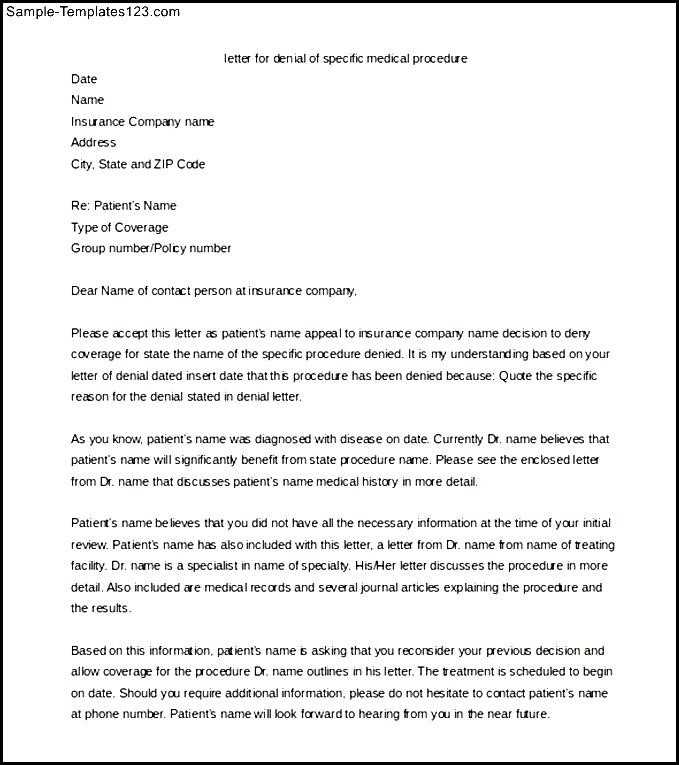
Start with a clear and concise statement that outlines the medical necessity of the requested service or treatment. Specify how the condition or diagnosis requires specific intervention for the patient’s well-being. Be precise in describing the medical condition and the direct link between the treatment and the patient’s health improvement.
Use supporting evidence from medical records or clinical guidelines to reinforce the claim. Highlight any tests, diagnoses, or previous treatments that demonstrate the need for the requested service. Provide details about how the patient’s condition affects their daily life and why alternative options are not suitable or effective.
Clearly identify the treatment or service being requested, along with the expected outcomes. This clarity helps insurance providers or decision-makers understand the direct benefits for the patient. Be specific about what makes this particular course of treatment medically necessary rather than just an option or preference.
Here’s the revised version, minimizing word repetition:
When crafting a medical necessity letter, focus on presenting clear and specific details. Avoid redundancy by stating the facts directly and supporting them with relevant medical data. Begin by outlining the patient’s condition and how the recommended treatment directly addresses their needs. Reference clinical studies or guidelines that align with the proposed treatment plan.
Specificity Over Redundancy
Clarify the diagnosis with concise language. Provide evidence of how alternative treatments have been ineffective or unsuitable. This reinforces the need for the requested intervention. Highlight the expected outcomes, using reliable medical sources to back your claims.
Support with Data
Whenever possible, use statistics or case studies to demonstrate the likelihood of success. This adds weight to the argument and avoids vague statements. Make sure to connect the patient’s unique circumstances with the scientific evidence available, ensuring the letter is tailored and not generic.
Maintain a professional yet accessible tone. Streamline the message, focusing on the necessary details to facilitate an understanding of the request. This increases the chances of the letter being reviewed and accepted quickly.
- Letter Medical Necessity Template
Start with a clear introduction that explains the patient’s condition and why the requested service or equipment is necessary. Focus on specific medical reasons that justify the need for the treatment. Outline the patient’s diagnosis and the associated symptoms that affect their daily life. Address how the condition limits their ability to perform regular activities.
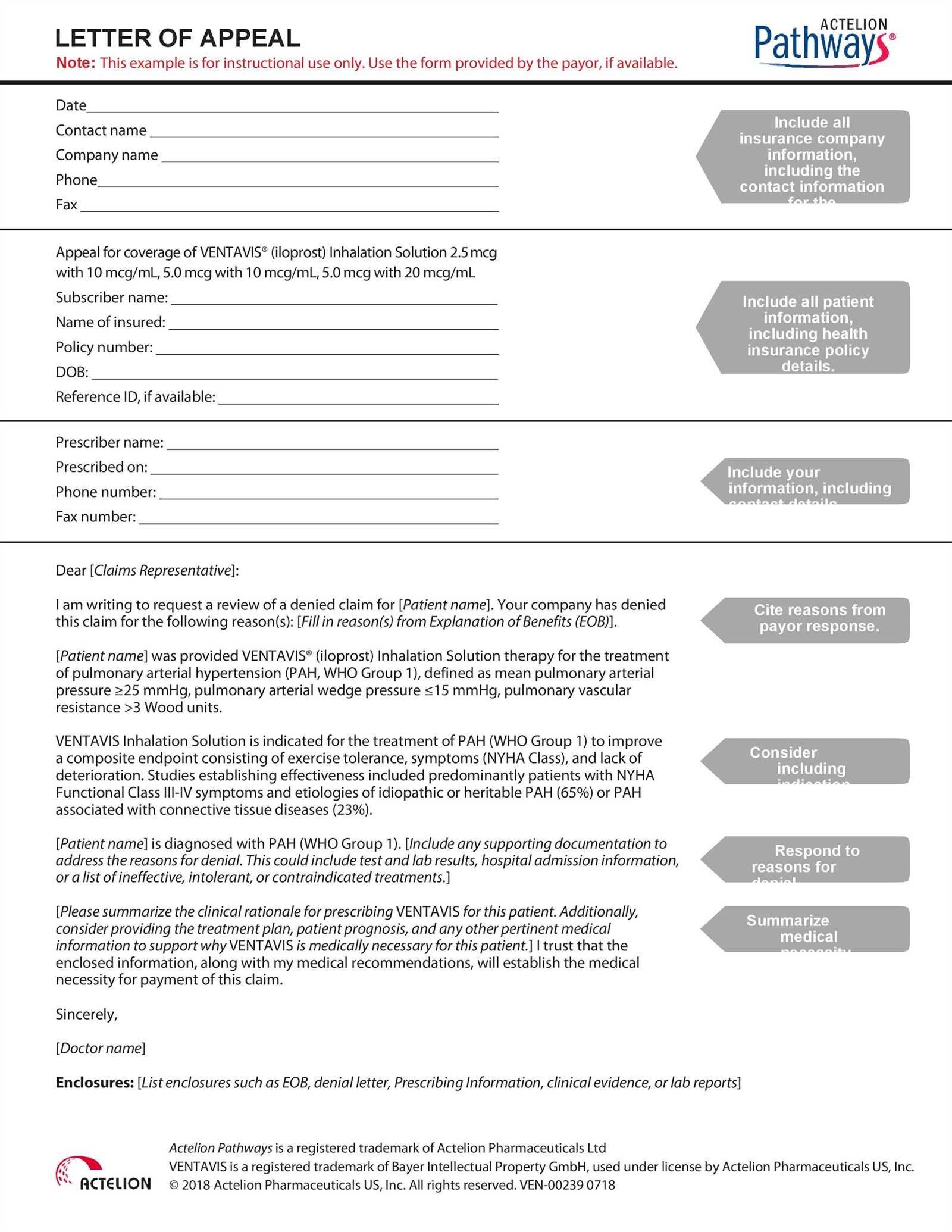
Step 1: Patient Information
Provide full patient details, including their full name, date of birth, diagnosis, and any relevant medical history. This allows the reader to understand the background of the case and ensures proper documentation.
Step 2: Explanation of Necessity
Clearly explain why the requested treatment, equipment, or service is medically necessary. Include the type of care required, whether it’s a specific medical device or ongoing therapy. Refer to clinical guidelines, studies, or professional opinions that support the recommendation. If applicable, describe other treatments the patient has already tried and why they were unsuccessful.
Conclude by reiterating the critical nature of the treatment and how it directly affects the patient’s quality of life. Use precise language to show why denying the request could lead to worsened health outcomes. Keep the tone firm yet professional, emphasizing the urgency and importance of timely approval.
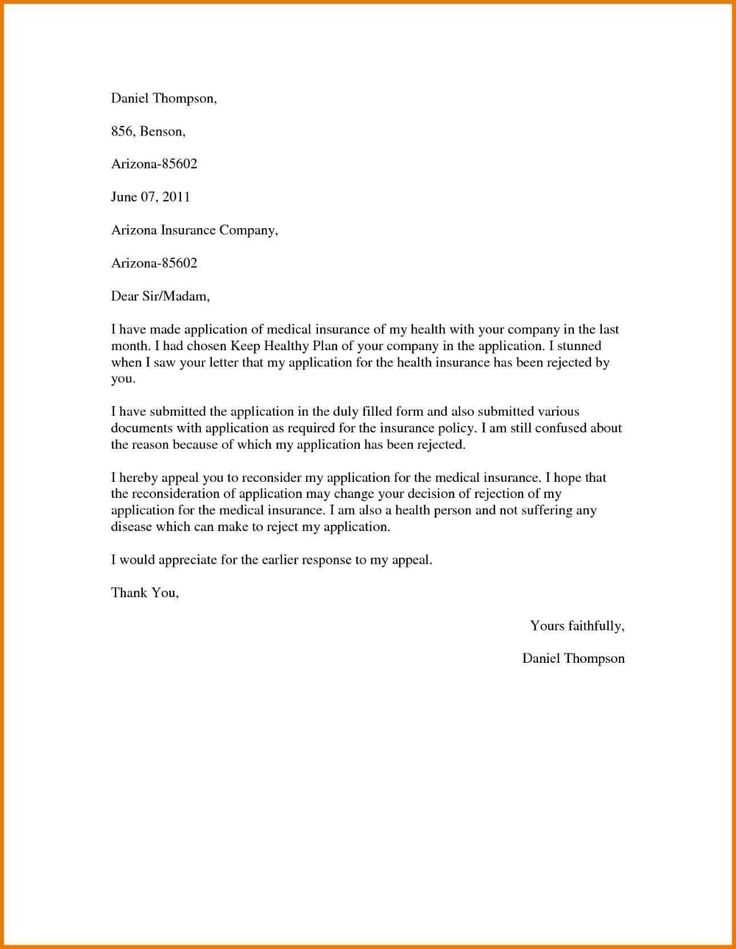
Begin with clear identification of the patient and their condition. Include the patient’s full name, date of birth, and insurance policy number. Follow this with a precise description of the medical condition, providing relevant diagnoses and symptoms. State how these affect the patient’s daily life and ability to function.
Detail the Treatment Plan
Outline the recommended treatment or service, specifying any procedures, medications, or therapies. Clarify how this treatment directly addresses the patient’s specific medical needs, including references to clinical guidelines or research supporting its use. Be concise but detailed enough to show that the treatment is the most appropriate option.
Provide Medical Rationale
Explain why the proposed treatment is necessary. Link it to the patient’s condition, emphasizing how it will improve their health outcomes or prevent further complications. Reference any previous treatments or interventions, explaining why they were insufficient or unsuccessful. Use medical terminology to convey the seriousness of the condition and the need for this specific intervention.
Justify the Timing: Stress the urgency of the treatment if applicable. Indicate how delays could worsen the patient’s condition, adding medical evidence or expert opinions to back your argument.
Conclude with a brief summary, reinforcing the medical necessity of the proposed treatment. Provide contact information for follow-up or additional details, and include your professional credentials, signature, and date.
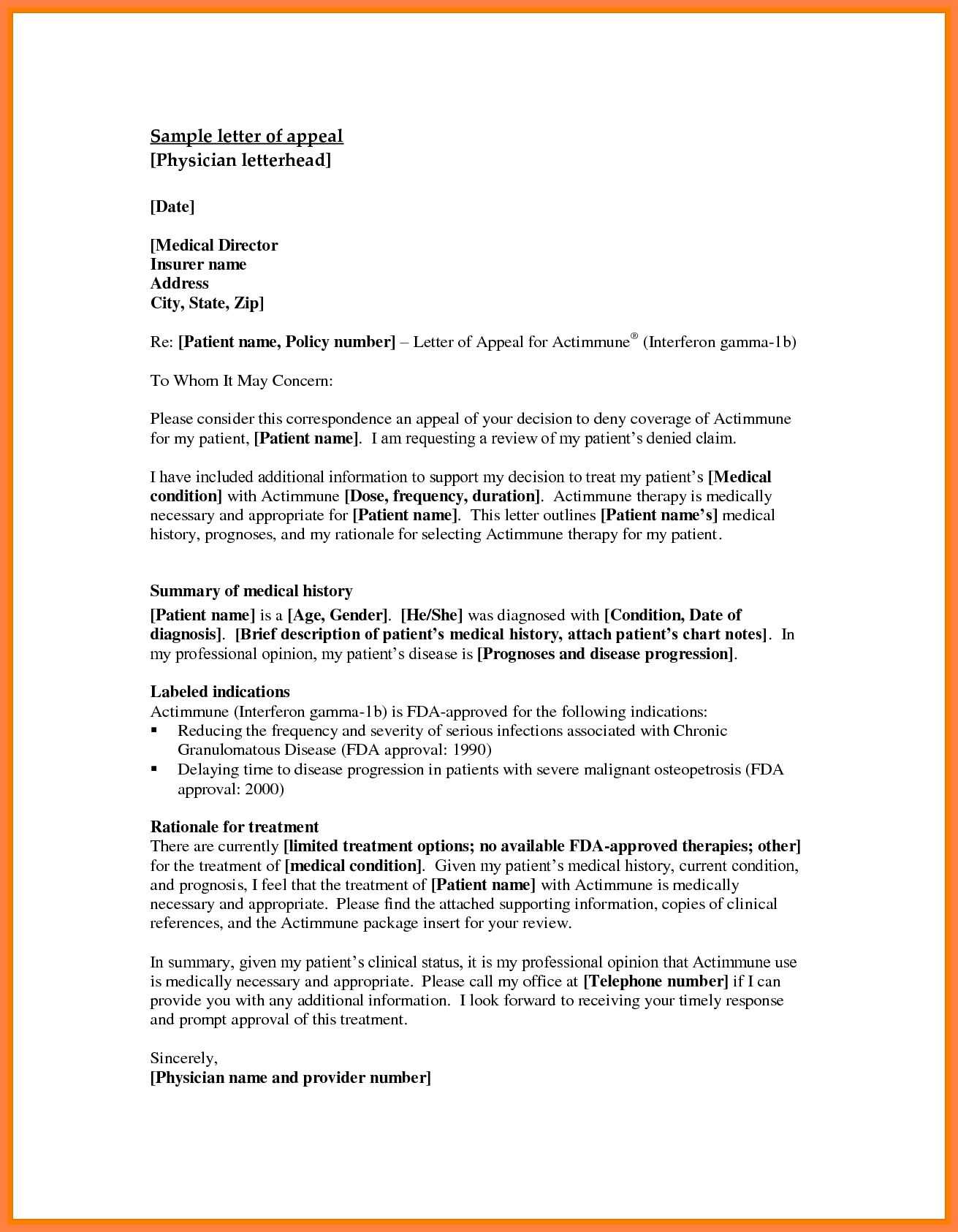
A medical necessity letter should present a clear, concise argument for why a specific treatment, procedure, or service is necessary for the patient’s health. The following key elements are critical to ensure the letter effectively communicates the need for the requested care.
1. Patient Information
Include the patient’s full name, date of birth, and insurance details. This ensures that the letter is directly linked to the correct individual and their specific health plan. Be sure to include contact information for the patient, if needed.
2. Diagnosis and Medical History
Provide a thorough description of the patient’s diagnosis. Include the medical history, current symptoms, and any previous treatments that have been tried. This contextualizes the need for the recommended service by highlighting the patient’s ongoing health challenges.
3. Description of Recommended Treatment
Clearly outline the treatment or service being requested. Specify why it is appropriate for the patient based on their unique condition. The letter should detail how the proposed solution addresses the patient’s specific medical needs and how it will improve their overall health outcome.
4. Supporting Evidence
Provide medical research, clinical guidelines, or expert opinions that support the necessity of the requested treatment. This can include studies or professional recommendations that demonstrate how the treatment is effective for the patient’s diagnosis.
5. Medical Provider’s Credentials
Include the medical provider’s qualifications, experience, and expertise in treating the specific condition. This lends credibility to the request and reassures the insurer that the recommendation comes from a knowledgeable professional.
6. Urgency of the Request
If applicable, explain why the treatment is urgent or time-sensitive. Highlight any risks associated with delaying the procedure or treatment, emphasizing the impact on the patient’s health and quality of life.
7. Contact Information
Include contact information for the medical provider so that the insurer can reach out for further details if needed. This should include phone numbers, email addresses, and any office hours during which the provider is available.
Each of these components will help to build a strong, persuasive case for the requested treatment and increase the likelihood of the request being approved.
To strengthen your medical necessity request, ensure that the details are accurate and clear. Avoid these common pitfalls:
- Vague or General Statements: Do not leave room for interpretation. Provide clear, specific evidence that supports the need for treatment. Instead of writing, “The patient requires therapy,” state, “The patient requires therapy due to chronic pain and muscle weakness, as evidenced by the following test results…”
- Failing to Provide Supporting Documentation: Always attach relevant medical records, test results, or physician notes. These documents back your claims and demonstrate the severity of the condition.
- Overlooking the Treatment’s Expected Outcome: Explain how the proposed treatment will benefit the patient’s health. Outline the improvements that can reasonably be expected, such as better mobility or reduced symptoms.
- Using Inappropriate Language: Stay professional and avoid using emotive language. Stick to the facts and avoid subjective descriptions that don’t contribute to the case.
- Not Addressing Insurance Requirements: Review your insurance provider’s medical necessity guidelines. Ensure the request aligns with their specific criteria and focuses on the treatments they consider necessary.
- Submitting an Incomplete Request: Double-check that all required information is included–date of diagnosis, physician’s credentials, detailed treatment plan, and cost estimates. Omitting any of these could delay the review process.
Final Steps to Avoid Mistakes
Before submission, proofread your request and check for clarity. Have someone else, such as a colleague or another healthcare professional, review the document. They may catch mistakes you overlooked.
Attach medical records that directly support the claims in your letter. These could include doctor’s notes, diagnosis reports, test results, and any other relevant medical history. Ensure that these documents are current and clearly show the medical necessity of the requested treatment or service.
Including letters from healthcare providers can strengthen your case. These letters should outline the specific reasons why the recommended treatment is necessary and how it will impact the patient’s health. A clear connection between the patient’s condition and the treatment should be made in the letter.
Make sure the documents are organized in a way that is easy to follow. Create a table summarizing key points from the attached documents, such as diagnosis, treatments tried, and the results. This makes it easier for the reviewer to see the progression of the patient’s condition and the rationale for the requested treatment.
| Document | Description | Relevance to Request |
|---|---|---|
| Doctor’s Letter | Details the patient’s medical history and treatment recommendations | Supports the need for the requested treatment based on the patient’s condition |
| Test Results | Lab results or imaging that confirm the diagnosis | Validates the diagnosis and shows the severity of the condition |
| Previous Treatments | Documentation of treatments that have been tried previously | Shows the progression of the condition and why further intervention is needed |
Be sure to redact any personal information not directly related to the request to protect privacy. This will also keep the focus on the medical necessity.
To increase the likelihood of approval, adjust the medical necessity letter based on the specific health plan’s requirements. Research the health plan’s coverage criteria and incorporate these details into the letter. For instance, some plans prioritize clinical guidelines, while others focus on cost-effectiveness or specific treatment protocols.
Provide evidence that aligns with the health plan’s coverage policy. If the plan requires proof of previous treatments, include relevant medical records, lab results, or imaging studies. For plans that emphasize the necessity of a treatment over alternatives, clearly explain why the recommended treatment is the only viable option for the patient’s condition.
Be specific about how the patient’s condition aligns with the health plan’s approved treatments. If the health plan outlines a step-by-step process for treatment approval, follow it precisely, addressing each criterion. Tailoring the letter to reflect these factors shows the health plan that the request is aligned with their approval process.
For plans with a focus on cost management, outline the long-term financial benefits of the proposed treatment. Highlight any preventive benefits or reduced future healthcare needs that may arise from the treatment. Including studies or data that show a cost-effective approach can make the letter more persuasive.
Finally, use clear, concise language and avoid generic or vague terms. Be direct in demonstrating how the treatment is medically necessary according to the specific health plan’s criteria. This will improve the chance of your letter being accepted and processed quickly.
Once you’ve submitted a medical necessity request, it’s important to track its progress and take the following steps to ensure timely approval and resolution.
- Follow up with the insurance company: Reach out to confirm that your request has been received. Keep a record of your communication for future reference.
- Review the details of your request: Double-check the supporting documents you’ve submitted to ensure they clearly outline the medical necessity and align with the insurer’s guidelines.
- Monitor any additional requests: The insurer may request more information or clarification. Respond to these requests promptly to avoid delays.
- Contact your healthcare provider: Keep your healthcare provider updated on the status of your request. They may need to provide additional support or documentation.
- Understand the timeline: Inquire about the typical timeline for approval or denial. Some insurers have specific time frames for processing requests, which can guide your follow-up schedule.
- Prepare for a possible denial: If your request is denied, ask for a clear explanation and understand the reasons behind it. You can then appeal the decision with additional evidence if necessary.
- Keep detailed records: Maintain a log of all interactions, including dates, names of representatives, and the outcomes of each communication. This will help you stay organized and be prepared in case of follow-up actions.
By staying proactive and organized, you can help speed up the process and ensure that the request is handled appropriately.
Now, each point minimizes the repetition of the keyword “Medical Necessity”.
Begin by clearly stating the necessity for the treatment or service in question. Define why the service is crucial for the patient’s health, based on medical evidence. This helps make the case for “Medical Necessity” by demonstrating that the proposed treatment directly addresses a diagnosed medical condition or urgent health issue.
1. Clinical Evidence
Present relevant clinical studies or guidelines that support the treatment’s effectiveness. Show how these studies apply to the patient’s specific condition to confirm the “Medical Necessity” of the treatment. Include comparisons to alternative treatments when applicable, proving the suggested approach is the most appropriate for the patient’s situation.
2. Patient’s Health History
Explain how the patient’s medical history aligns with the treatment. Provide a clear connection between past conditions, symptoms, and the need for a specific intervention. This reinforces the “Medical Necessity” by indicating that the patient’s individual health status requires this particular approach.
3. Expected Outcomes
Outline the expected health improvements resulting from the treatment. Be specific about how the intervention will directly impact the patient’s well-being. Highlight measurable outcomes that can justify the “Medical Necessity” for coverage, particularly focusing on quality of life or prevention of further health complications.
4. Alternatives and Rationale
Discuss other available treatments and explain why they are less appropriate or insufficient. Clarify how the recommended treatment surpasses alternatives in addressing the patient’s health needs. This comparison strengthens the argument for “Medical Necessity” by eliminating other options that may not be as effective or suitable.