Prescription letter template
Creating a prescription letter requires attention to detail and clarity. The template you choose should reflect professionalism while ensuring the necessary information is presented in an organized manner. A well-structured letter minimizes confusion and provides the recipient with a clear understanding of the prescribed treatment.
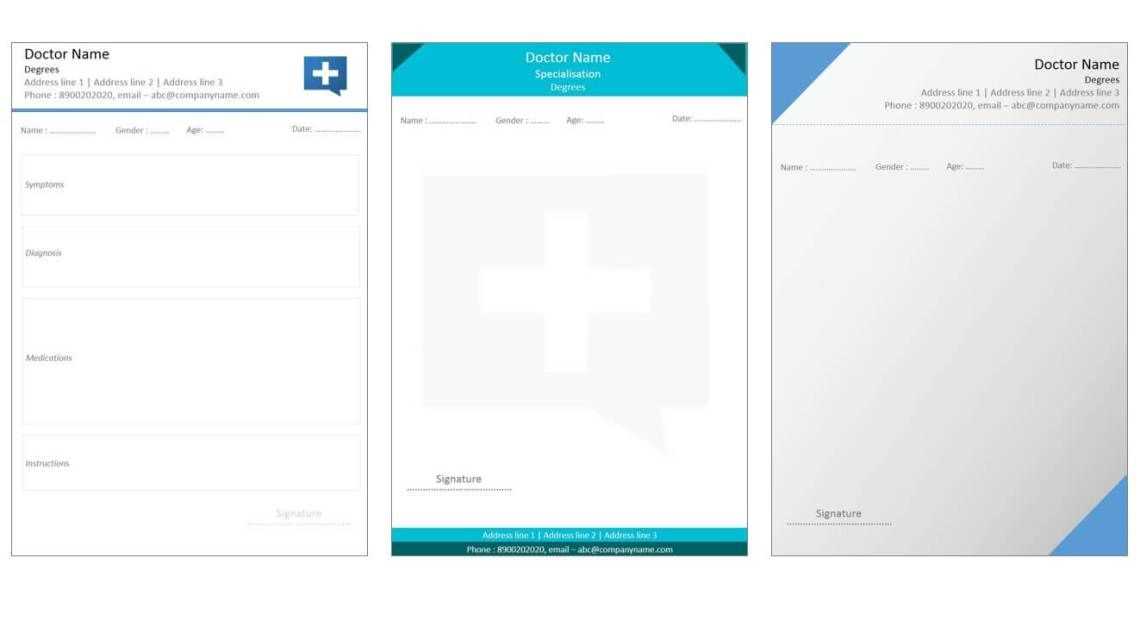
Start with a header that includes your full name, title, contact information, and the date of issuance. This ensures the letter has all the required identification details from the start. In the body, clearly state the patient’s name, their medical condition, and the specific medication or treatment prescribed. Make sure to include dosage instructions, frequency, and any necessary follow-up care.
Don’t forget to include your signature at the end of the letter, along with any relevant credentials. This adds authority to the prescription and helps avoid misunderstandings. Keeping the letter concise and professional will improve its overall effectiveness.
Here’s a version without word repetition:
Focus on clarity and precision when drafting prescription letters. Keep sentences short and to the point. Avoid over-explaining details. Instead, provide only the most necessary information in a structured format.
Structure the Letter
Start with patient identification and contact details. Follow with diagnosis and prescribed medication. Include dosage, frequency, and duration for proper treatment.
Information to Include
| Section | Description |
|---|---|
| Patient Details | Full name, date of birth, and contact information. |
| Diagnosis | Clear explanation of the condition requiring treatment. |
| Medication | Details of prescribed drugs, including dosage and method of administration. |
| Duration | How long the treatment should last. |
End the letter with your signature and professional credentials. This ensures a smooth and clear communication between healthcare providers and patients.
- Prescription Letter Template
Begin by clearly stating the patient’s full name and their date of birth. Indicate the specific medication prescribed, its dosage, and the duration for which it should be taken. Be sure to include the reason for the prescription, whether it’s for a chronic condition or a temporary issue. Ensure that the letter contains any relevant instructions regarding the use of the medication, such as how often it should be taken, whether it should be consumed with food, and any possible side effects the patient should monitor.
Next, provide the prescribing doctor’s full name, medical qualifications, and contact information. This adds credibility and ensures that the patient or pharmacy can reach out for any necessary clarifications. The letter should also include the doctor’s signature and the date of issuance, confirming the validity of the prescription.
Finally, it is beneficial to include any additional notes or precautions for the patient’s safety. If there are any follow-up appointments or tests required, mention them. A clear and concise prescription letter can prevent confusion and provide the necessary information to ensure the patient receives the correct treatment.
Begin with the header that includes your contact information, including your name, professional title, address, phone number, and email. This should be aligned to the top left of the letter, allowing easy access to your details. Below that, include the date the letter is being written.
Next, add the recipient’s details. This section should contain the patient’s full name, address, and any other relevant contact information. Ensure this section is properly aligned with your header for clarity and consistency.
For the salutation, address the recipient respectfully, such as “Dear [Patient’s Name]” or “To Whom It May Concern,” depending on the nature of the letter. Follow with a clear introduction that specifies the purpose of the prescription letter, indicating the medication prescribed and any dosage instructions. Be concise yet thorough to avoid ambiguity.
The body of the letter should outline specific treatment details, including medication names, dosages, frequency of intake, and any special instructions related to administration or duration. It is helpful to include any known side effects or warnings associated with the prescribed drugs to ensure the patient is fully informed.
Conclude the letter with a polite closing statement that encourages the patient to reach out with any questions. Sign off with your name, title, and any additional credentials. If necessary, you can also include the date of your signature and a contact method for follow-up.
Lastly, review the letter for clarity, accuracy, and any medical or grammatical errors to ensure it is professional and reliable.
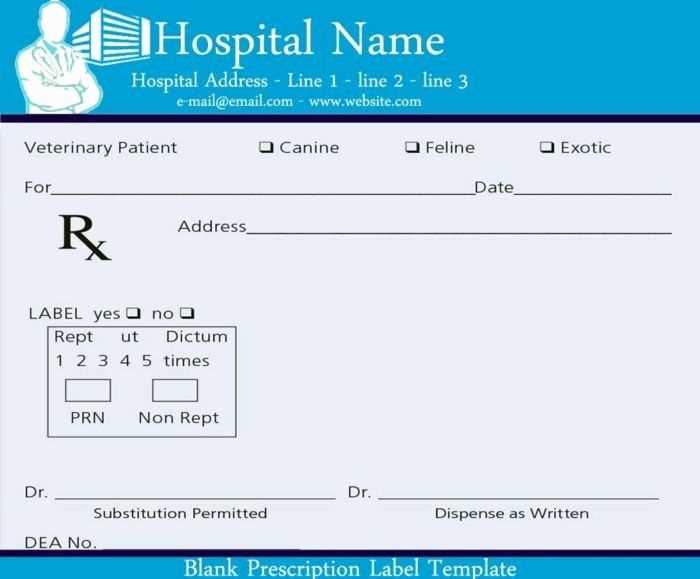
Include the patient’s full name and date of birth. This helps identify the recipient and avoids any confusion regarding medication orders.
Clearly specify the medication name, including the dosage, frequency, and form (e.g., tablet, liquid). Use precise terms to avoid errors in interpretation.
State the quantity of the prescribed medication and the total number of refills allowed, if any. This ensures the pharmacy dispenses the right amount and the patient knows how long the prescription lasts.
Indicate any specific instructions for the patient, such as whether the medication should be taken with food or any potential side effects to watch for. This promotes safe use of the medication.
Provide your signature, medical license number, and contact details. This information is required for the prescription’s legitimacy and for the patient or pharmacy to reach out if needed.
| Information | Details |
|---|---|
| Patient’s Information | Full name, Date of birth |
| Medication Details | Name, Dosage, Form, Frequency |
| Quantity & Refills | Amount of medication, Number of refills |
| Instructions | Special instructions for use, Side effects |
| Signature & Contact | Physician’s signature, Medical license number, Contact details |
When writing a prescription letter, clarity and accuracy are paramount. Avoid these common mistakes to ensure your letter serves its purpose effectively.
1. Incorrect Patient Information
Double-check the patient’s name, date of birth, and contact details. An error here could lead to confusion or delays in treatment. Make sure all information matches the medical records accurately.
2. Unclear Medication Instructions
Specify the medication dosage, frequency, and method of administration clearly. Ambiguous instructions can lead to misinterpretation and potential harm. Always be specific about the treatment regimen.
3. Failure to Include Relevant Medical History
Provide important background information, such as allergies or pre-existing conditions, that could influence the treatment. Omitting this can affect how the prescribed medication interacts with the patient’s health.
4. Incomplete Signature or Credentials
Ensure your signature is present along with your professional title and license number. An unsigned letter or missing credentials may render the prescription invalid or questionable.
5. Ambiguous Language or Jargon

Avoid using complex medical terms or abbreviations that might confuse the reader. Use clear, simple language to ensure the prescription is easily understood by both the patient and the pharmacist.
6. Lack of Follow-Up Information
Clearly mention how often follow-up appointments should occur or when the next check-up is due. This ensures continuity in care and helps track the effectiveness of the prescribed medication.
7. Forgetting to Include the Date
Always include the date the prescription was written. This is essential for record-keeping and verifying the prescription’s validity.
8. Incorrect Format
Stick to a clear, professional format. Avoid cluttering the letter with unnecessary details. A well-organized prescription letter is easier to read and process.
When adapting a prescription for different medications, it’s critical to adjust the details based on the specific drug’s requirements and patient needs. Each medication has unique dosage instructions, potential interactions, and administration methods that need clear communication on the prescription. Here’s how to approach the adaptation process effectively:
- Adjust Dosage Instructions: Tailor the dosage based on the patient’s condition and the medication’s strength. For example, some medications require a slow titration of the dose, while others might need to be given in divided doses throughout the day.
- Note the Formulation: Medications come in various forms, such as tablets, liquids, or injections. Specify the correct form based on the patient’s preferences, age, and any difficulties they may have with swallowing pills or handling specific formulations.
- Incorporate Administration Guidelines: Some drugs need to be taken with food, while others should be taken on an empty stomach. Indicate this clearly to avoid adverse effects or reduced efficacy. If a medication requires refrigeration or special handling, include this in the prescription.
- Account for Drug Interactions: Verify that there are no harmful interactions between the prescribed medication and any other drugs the patient is currently taking. Adjust the dosage or frequency if necessary to prevent complications.
- Consider Patient-Specific Factors: Take into account the patient’s age, weight, renal function, and comorbid conditions when adapting a prescription. Some medications require lower doses for elderly patients or those with kidney issues.
- Provide Clear Refill Instructions: Depending on the medication, you may want to specify whether refills are allowed, and if so, how many. For controlled substances, this information is critical and should be indicated per legal requirements.
Adjusting a prescription to fit the specifics of each medication ensures the patient receives the correct treatment, reducing the risk of errors and enhancing therapeutic outcomes.
Always sign the prescription letter in a clear and legible manner. Use a consistent signature that is easily identifiable. Avoid using digital signatures unless explicitly allowed by your institution or local regulations.
1. Verify Patient Information
- Ensure that the patient’s full name, date of birth, and other personal details are correct before signing.
- Double-check any medical conditions or history noted in the prescription.
- Confirm that the prescribed medication aligns with the patient’s current treatment plan and medical history.
2. Confirm Prescription Details
- Double-check the drug name, dosage, route, and frequency.
- Ensure the duration of the medication course is clearly specified.
- If applicable, include additional instructions for administration or handling.
Once verified, include your credentials–such as your professional title and registration number–on the prescription to confirm your authority.
3. Use Secure and Legal Methods
- Follow the required legal format for prescriptions as outlined by your local medical authority.
- Consider including a security feature such as a unique prescription number to prevent tampering.
After signing, always provide the patient with a clear copy and ensure proper documentation is kept for your records. This helps safeguard against potential legal or medical issues down the line.
Prescription letter templates must comply with specific legal standards to ensure their validity and prevent misuse. Accurate patient information, correct prescribing details, and the appropriate signatures are fundamental components in creating legally sound prescription letters.
Data Protection and Confidentiality
Prescription letters contain sensitive patient data, so it’s crucial to protect that information. Compliance with data protection laws, such as GDPR in the EU or HIPAA in the US, is required to prevent unauthorized access or breaches. Always ensure that personal health information is stored securely, and only authorized parties have access to it.
Legal Validity and Signatures
In many jurisdictions, a prescription letter must be signed by a licensed healthcare provider to be legally recognized. Electronic signatures are gaining acceptance in various regions, but they must meet specific standards and regulations for authenticity. Double-check that your template includes space for the necessary signatures, including those from the prescribing doctor or authorized personnel.
Ensure your prescription letter is clear and concise by following a straightforward structure. Begin with the patient’s full name and their birthdate to confirm their identity. List the diagnosis or condition being treated, along with the prescribed medication or treatment plan. Always include the exact dosage and any special instructions to avoid confusion. If applicable, specify the duration of the treatment or prescription refills.
Key Points to Include:
- Patient Information: Name, date of birth, and any relevant medical record numbers.
- Diagnosis: Clear description of the medical condition being treated.
- Medication Details: Name, dosage, frequency, and duration of the medication.
- Additional Instructions: Include any necessary details for administration or adjustments.
Be sure to include your contact information and signature at the end of the letter for verification purposes. This will allow healthcare providers to reach out if any clarifications are needed. If you’re prescribing a controlled substance, follow all legal requirements for documentation.