Discharge letter from medical practice template
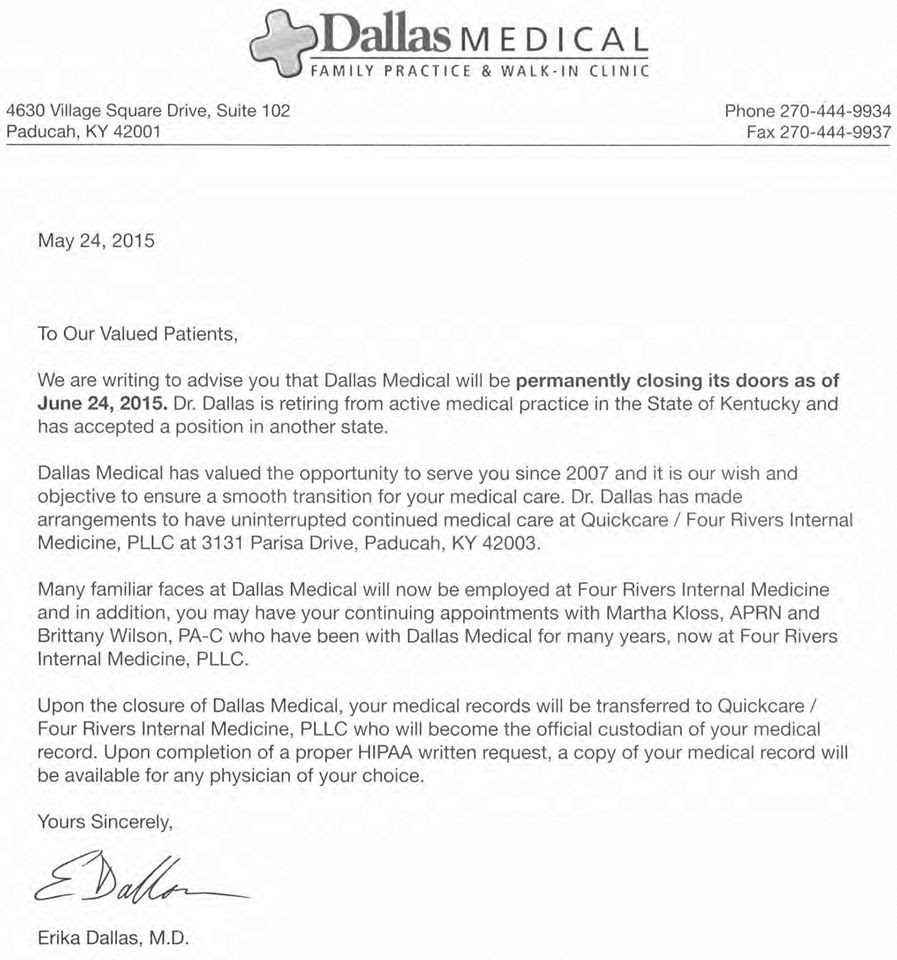
To create a professional discharge letter, ensure you follow a clear and concise structure. Start by addressing the patient directly, acknowledging their time under your care and outlining the key details of their discharge. Mention the effective date of the discharge and any important instructions regarding follow-up care or further steps the patient should take. It’s also helpful to include a brief summary of the treatment provided and any specific health recommendations moving forward.
Use simple, direct language to avoid confusion. If the patient requires ongoing care from another provider, include relevant contact details or any necessary referrals. Make sure the tone remains courteous, providing reassurance and expressing gratitude for their cooperation throughout their treatment.
Clarify any discharge instructions that are critical for the patient’s well-being, such as medication, physical activity restrictions, or follow-up appointments. Ensure all necessary contact information for your practice or the referred medical professionals is easy to find, and offer the patient resources for additional support if needed.
Here’s the corrected version:
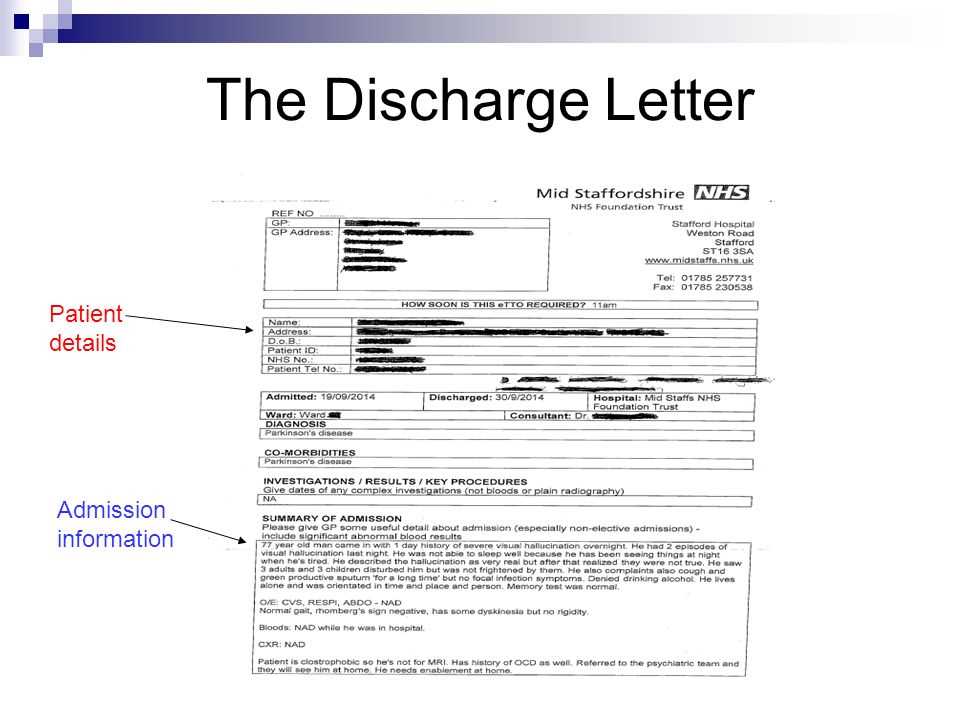
Ensure that the discharge letter is clear and concise. Provide the patient’s name, date of discharge, and reason for leaving the practice in the opening lines.
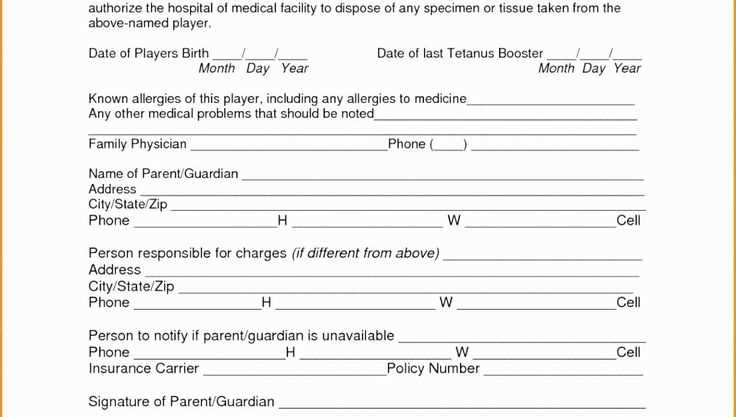
- Patient Information: Include full name, date of birth, and patient ID number if applicable.
- Discharge Date: State the exact date of discharge to avoid any confusion.
- Reason for Discharge: Briefly mention why the patient is leaving the practice, whether due to a completed treatment or change of healthcare provider.
Ensure the letter reflects the patient’s medical history briefly, mentioning key treatments, results, or progress during their time with the practice. Also, be transparent about any necessary follow-up care or recommendations for further treatment.
- Follow-Up Care: Clearly outline any follow-up visits, recommended treatments, or referrals.
- Additional Instructions: If applicable, provide information on ongoing prescriptions or future medical needs.
Conclude by thanking the patient for their trust and offering contact information for any future inquiries or needs. End the letter with a professional sign-off and your practice’s details for easy reference.
- Discharge Letter from Medical Practice Template
A discharge letter from a medical practice serves as a formal notification to a patient that they are being released from care. It should be clear, concise, and provide all relevant details for a smooth transition. Below is a template you can use for drafting a discharge letter.
Discharge Letter Template
Dear [Patient’s Name],
This letter serves as notification that your care at [Medical Practice Name] is concluding as of [Date]. We have successfully addressed your treatment needs, and based on your progress, we are confident that you no longer require further care under our services.
If you have any questions or require additional information, please do not hesitate to contact our office. We recommend that you follow up with [Name of Primary Care Physician/Specialist] for continued care, or consult with another healthcare provider should you need further attention.
We have included a summary of your treatment, any follow-up appointments or prescriptions, and any additional instructions below:
- Summary of Treatment: [Detailed Summary]
- Follow-up Appointments: [Date/Time/Location]
- Prescriptions: [List of Medications, Dosage, and Instructions]
- Special Instructions: [Any Additional Care Instructions]
We appreciate the trust you have placed in our practice, and we wish you the best in your continued health. If you require any further assistance, please reach out at [Phone Number] or [Email Address].
Best regards,
[Your Name]
[Your Title]
[Medical Practice Name]
[Contact Information]
To create a thorough discharge letter, focus on these components:
- Patient’s Information: Include the patient’s full name, date of birth, and any relevant identification numbers to ensure clarity.
- Discharge Date: Clearly state the official discharge date to avoid any confusion regarding the patient’s status.
- Reason for Discharge: Briefly describe the reason for the patient’s discharge, whether due to recovery, treatment completion, or transfer to another facility.
- Instructions for Post-Discharge Care: Detail any follow-up care, medications, or lifestyle changes the patient needs to adhere to. Be specific about appointment dates, medication dosage, and any referrals made.
- Doctor’s Contact Information: Include the contact details of the medical provider responsible for the patient’s care. This ensures the patient can reach out for any questions or concerns after discharge.
- Summary of Treatment and Care: Provide a summary of the treatment plan that was followed, including tests performed, diagnoses made, and procedures done during the patient’s stay.
- Final Assessment: A concise evaluation of the patient’s condition at the time of discharge, along with any notes regarding expected recovery or ongoing health issues.
Each of these sections is important for a well-rounded discharge letter that facilitates smooth transition and continuity of care.
Tailor the letter by using the patient’s name throughout the document. Begin with a warm greeting, such as “Dear [Patient’s Name],” to establish a personal connection. Include specific details about their treatment, recovery progress, and any unique aspects of their care. Mention milestones they’ve achieved or any challenges they’ve overcome, showing that you recognize their efforts. Refer to their treatment plan or future steps, highlighting how it relates to their individual needs.
Be sure to include relevant instructions or recommendations specific to the patient’s situation. For example, if they require follow-up care, provide clear dates or steps that will help them stay on track. Avoid generic phrases and instead focus on their particular circumstances. This adds a personal touch that makes the letter feel unique to them.
Conclude with a personalized sign-off, such as “Wishing you continued health, [Your Name],” and ensure the letter’s tone is consistent with the rapport you’ve established with the patient during their care. This small detail can leave a lasting impression and reinforce the trust you’ve built throughout their treatment.
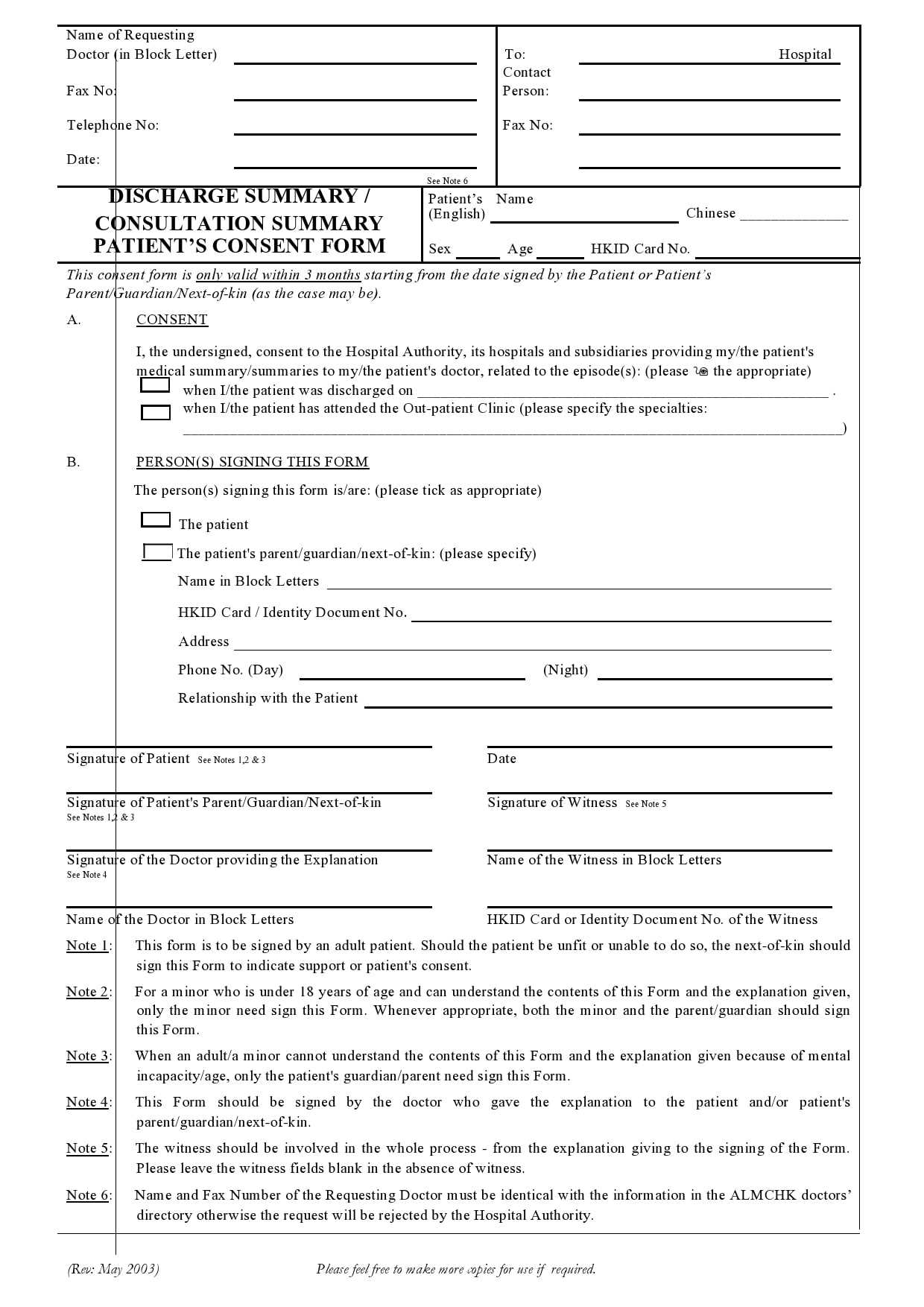
Discharging a patient must be done with careful attention to legal requirements to avoid potential malpractice or litigation risks. It is vital to ensure that the discharge is clear, documented, and in compliance with the laws of your jurisdiction.
Documenting the Discharge Process
Proper documentation plays a key role in protecting healthcare providers. Ensure the discharge decision, instructions, and any follow-up care details are recorded in the patient’s medical record. Include the rationale for discharge, any instructions for aftercare, and confirmation that the patient understood these instructions. This documentation helps mitigate risks if a dispute arises over the discharge process.
Patient Understanding and Consent
Before discharge, confirm that the patient understands their medical condition, the reasons for discharge, and any instructions for aftercare. Obtain verbal or written consent from the patient, acknowledging their understanding. In case of any language or comprehension barriers, provide the necessary support to ensure clarity.
Discharge Against Medical Advice (AMA)
If a patient chooses to leave the facility against the recommendation of their healthcare provider, this must be documented in the patient’s record. The provider should clearly explain the risks of leaving early and make every effort to ensure the patient understands. A signed AMA form helps protect the provider from future claims, indicating the patient was fully informed of the potential consequences.
Special Considerations for Vulnerable Populations
Patients with mental health issues, cognitive impairments, or other vulnerabilities require additional care during discharge. In these cases, ensure a caregiver or family member is involved in the discharge process and that the patient has appropriate support. Failing to provide this can lead to legal complications if the patient’s condition deteriorates after discharge.
Legal Requirements for Follow-Up Care
Provide clear follow-up instructions for any necessary care or appointments. Some jurisdictions require healthcare providers to ensure that patients receive timely follow-up care after discharge. Failure to comply with these requirements may lead to claims of negligence if the patient’s condition worsens.
Table: Key Legal Actions for Discharge
| Action | Legal Requirement | Recommendation |
|---|---|---|
| Documentation of Discharge | Ensure all actions, patient instructions, and consents are clearly recorded. | Maintain detailed records in the patient’s file. |
| Patient Consent | Document patient’s understanding and agreement. | Have the patient sign an acknowledgment of discharge instructions. |
| Discharge AMA | Document patient’s decision to leave against medical advice. | Provide a clear explanation of the risks involved and obtain a signed AMA form. |
| Follow-Up Care | Provide clear instructions for any necessary follow-up visits. | Ensure the patient has appointments or arrangements for care post-discharge. |
Legal risks can be minimized by adhering to clear, well-documented procedures and ensuring the patient’s rights and understanding are respected throughout the discharge process.
One common mistake is failing to provide clear and concise information about the patient’s current health status. Make sure to include specific details, such as treatment outcomes, ongoing care recommendations, and any follow-up steps needed. Avoid vague phrases like “doing better” without concrete evidence.
1. Leaving Out Key Information
Omitting essential details, like the patient’s diagnosis or medications prescribed, can confuse the reader and delay proper care. Include all relevant medical information that will assist the next healthcare provider in continuing treatment effectively. Always double-check if any crucial points have been missed.
2. Using Unprofessional Language
Stay professional and avoid casual or overly complex language. Using informal terms or overly technical jargon can cause misunderstanding. Aim for clarity and professionalism, ensuring the letter is easily understood by the receiving medical staff.
3. Making Assumptions About the Reader’s Knowledge
Do not assume that the reader has prior knowledge of the patient’s case. Provide enough background information so they can understand the context of the treatment and the patient’s condition. It’s essential to avoid any assumptions that may cause confusion.
4. Incorrect Formatting
Proper formatting makes the letter easier to read and ensures that important information is not overlooked. Avoid long paragraphs, and consider using bullet points or headings to organize the details logically. This allows the reader to quickly find key facts about the patient’s health.
5. Ignoring Privacy Concerns
Always be mindful of patient confidentiality. Avoid sharing any sensitive personal details not directly related to medical care. Adhere to privacy regulations like HIPAA to protect the patient’s personal and medical information.
Specify the next steps clearly, including any follow-up appointments, tests, or treatments. Include the date, time, and location of the next appointment, or instructions on how the patient can schedule it if not already arranged. Provide details on the purpose of follow-up visits and what the patient should expect, such as any tests to be conducted or changes to treatment plans.
Highlight any signs or symptoms to watch for that may require immediate attention, and give the patient clear instructions on what to do if those symptoms occur. If the patient needs to make lifestyle changes, mention these as part of the recovery process and suggest resources or support for assistance.
Ensure contact information for follow-up inquiries is included, as well as any forms or documents needed for the next visit. If any referrals or specialist visits are required, include those details with guidance on how to proceed.
Send the discharge letter as soon as possible after the patient is discharged. This ensures that the patient has all the necessary information in a timely manner. Make sure the letter is clear, concise, and free of medical jargon, so the patient can easily understand the details. Double-check the accuracy of the information before sending it, as errors can lead to confusion and potential complications.
Use the Right Medium
Choose a delivery method that suits the patient’s preferences. If the patient prefers email, make sure to use a secure platform. For those who prefer traditional methods, mailing a physical copy may be more appropriate. Always confirm the delivery method with the patient to avoid delays or missed communication.
Include Clear Follow-up Instructions
Ensure the discharge letter includes any follow-up care instructions, including appointments, medication schedules, and potential symptoms to watch for. If there are any specific actions the patient needs to take, clearly state them. This helps the patient manage their care post-discharge and reduces the chances of readmission.
So, I slightly rearranged the phrases to avoid repetitions.
To ensure clarity and reduce redundancy in your discharge letter, focus on rephrasing similar statements. This method helps maintain the letter’s readability and prevents the repetition of key points, making the overall tone more professional and concise.
Rephrasing Key Points
Instead of repeating the same phrase, try to vary the wording while keeping the message intact. For example, if you need to convey that the patient is recovering well, instead of saying “The patient is recovering well” multiple times, you can rephrase it as “The patient is making good progress” or “Recovery is proceeding as expected.” These subtle changes keep the text fresh and engaging.
Maintain Consistent Tone
While avoiding redundancy, ensure that the overall tone of the letter remains consistent. Make sure that you maintain a professional, supportive, and clear style throughout the document. Avoid switching to overly formal or too casual language, as this can confuse the reader.