Letter of Medical Necessity for Medication Template
When seeking approval for a specific treatment or therapy, it’s crucial to provide the appropriate documentation to demonstrate why the prescribed approach is essential. This type of correspondence plays a pivotal role in convincing healthcare providers and insurance companies to approve certain treatments or drugs. It highlights the medical need and justification for why a particular solution is required for the patient’s well-being.
Creating a structured and clear request is key. By following a well-organized format, individuals can present the necessary information in a professional and concise manner, making it easier for decision-makers to understand the urgency and importance of the request. This ensures that the treatment plan is both supported and prioritized.
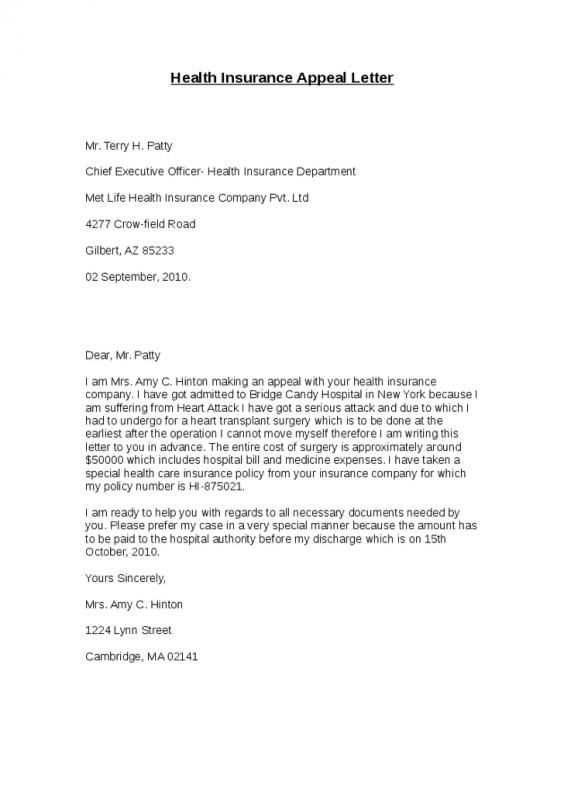
Properly drafted requests are often critical to navigating insurance hurdles and ensuring patients receive the care they require. Whether the request is for a specific drug or a particular type of care, clarity and precision are essential to avoid delays or rejections.
Understanding Medical Necessity Letters
In healthcare, certain documents are required to justify the need for specific treatments or therapies. These documents serve as formal requests to healthcare providers or insurance companies, ensuring that necessary interventions are approved. Their purpose is to provide detailed evidence supporting the importance of a prescribed solution, highlighting the urgency and relevance of the requested service.
Key Components of a Support Request
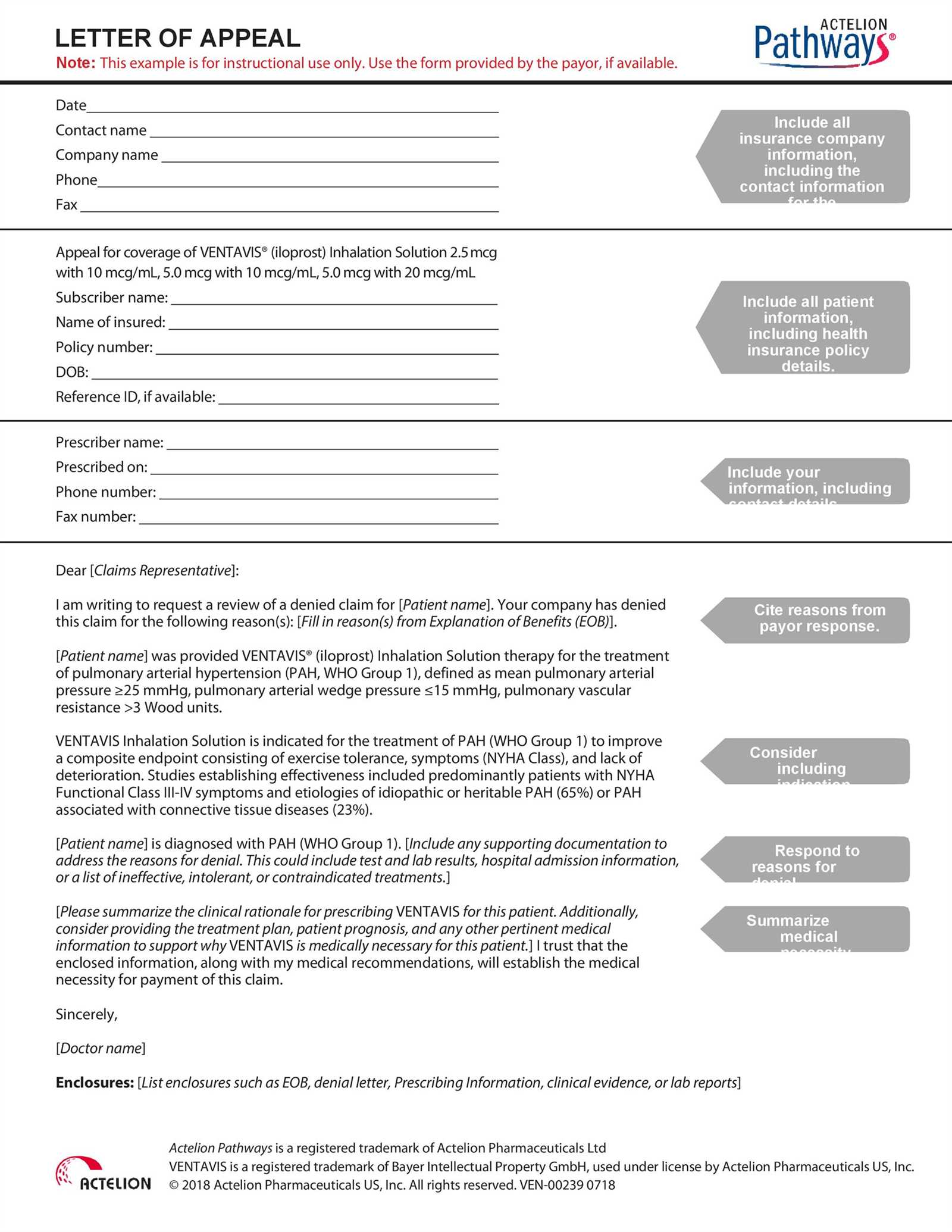
A well-structured request document typically includes several essential components. These elements help establish the medical necessity of the treatment and provide a solid foundation for approval. Some of the key components include:
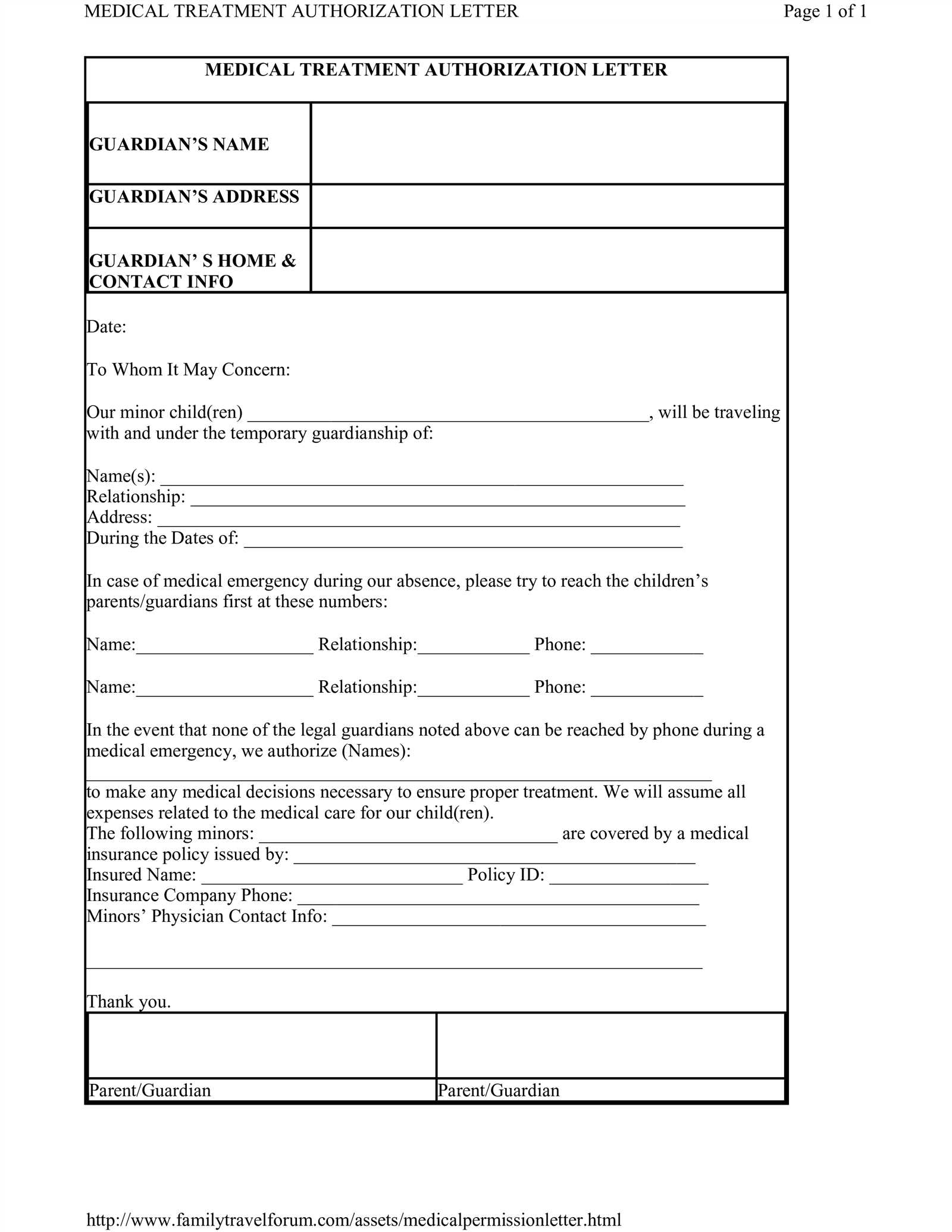
- Patient Information: Essential details about the patient, including medical history and current condition.
- Treatment Justification: A clear explanation of why the proposed therapy or drug is crucial for the patient’s health.
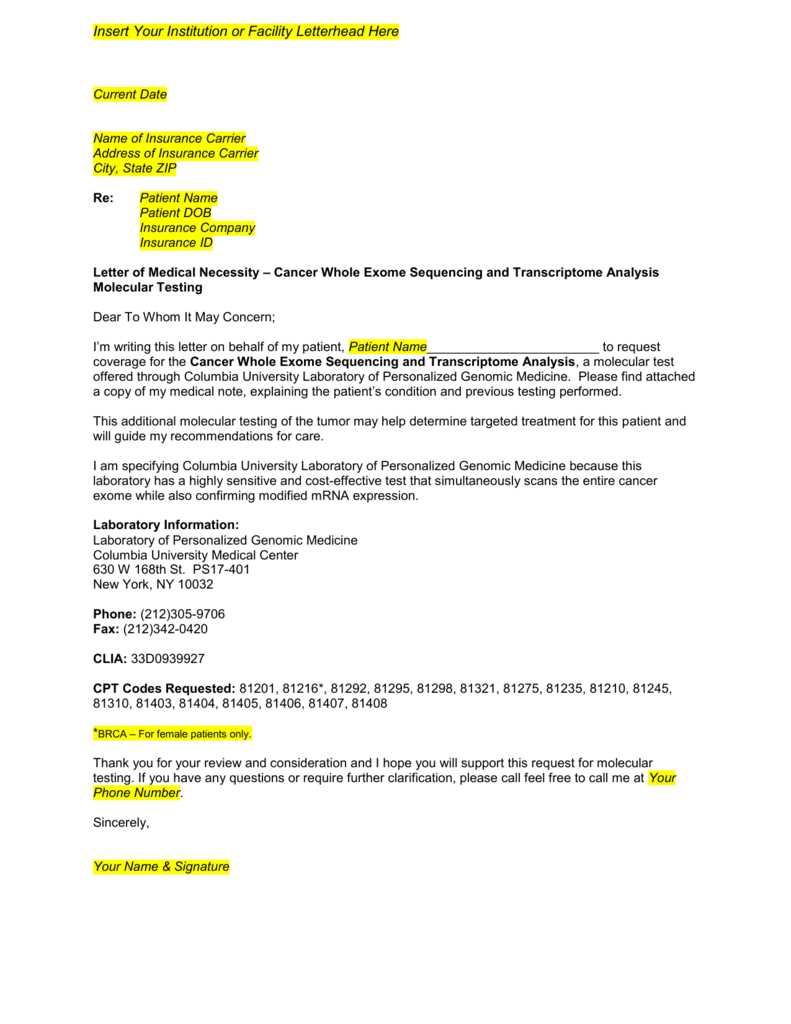
- Supporting Documentation: Any relevant test results, medical reports, or previous treatment records that validate the need for the requested intervention.
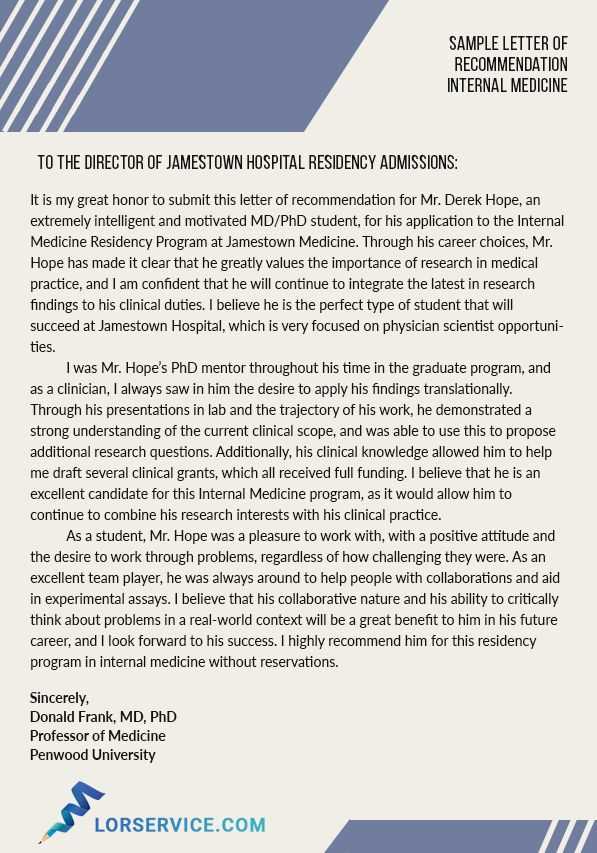
- Physician’s Recommendation: A statement from the healthcare provider endorsing the proposed course of action.
Why These Documents Are Crucial
These types of formal documents are essential for ensuring that patients receive the right care at the right time. Without a properly drafted request, patients might face delays, rejections, or the inability to access necessary treatments. By clearly outlining the medical justification, these requests make it easier for the intended recipients to understand why the proposed solution is critical and why it should be approved.
Why You Need a Template for Medication Requests
Having a well-organized structure for submitting treatment requests is essential when seeking approval from healthcare providers or insurers. Using a predefined structure can save time and ensure that all necessary information is included. A consistent format reduces the risk of missing important details and helps streamline the approval process.
With a ready-made format, individuals can focus on providing the essential medical justification rather than worrying about the layout or order of information. It simplifies the process of crafting a formal request, making it easier to gather the right data and ensure that the request meets the standards required by insurers or healthcare professionals.
Key Elements to Include in Your Request
To ensure a successful outcome when submitting a treatment request, it’s important to include specific details that clearly outline the necessity of the proposed solution. Each section of the document should serve a purpose, helping healthcare providers or insurance companies quickly assess the validity and urgency of the request.
Here are some of the essential elements to include:
- Patient Identification: Basic details about the patient, such as name, age, and medical history, to provide context.
- Condition Description: A thorough explanation of the patient’s current condition and how it affects their daily life or health.
- Proposed Treatment: Detailed information about the recommended treatment or therapy, explaining its relevance and why it is necessary.
- Supporting Evidence: Relevant test results, medical reports, or professional opinions that back up the proposed plan.
- Physician’s Endorsement: A statement from the prescribing physician confirming the need for the treatment and its expected outcomes.
How to Customize the Template for Your Needs
Once you have a basic framework for submitting treatment requests, it’s important to personalize the document to match the specific details of the patient’s case. Customizing the content ensures that the request accurately reflects the individual’s health condition, treatment requirements, and the necessary supporting evidence.
Adjusting the Content Based on the Patient’s Condition
The first step in customizing is to tailor the text to the patient’s unique health situation. This includes describing the patient’s medical history, the severity of their condition, and the specific symptoms that justify the proposed treatment. The more detailed and relevant the information, the stronger the case for approval.
Incorporating Relevant Medical Documentation
Ensure that the request includes all necessary medical documents such as test results, lab reports, and expert opinions. By integrating this supporting evidence into the request, you strengthen the argument for why the suggested treatment is crucial. Personalizing the content by including specific data related to the patient’s condition helps make the case more compelling.
Common Mistakes to Avoid When Writing
When preparing a formal request for treatment, it’s essential to avoid common errors that can weaken the argument or cause delays. Small mistakes in the presentation, content, or structure can lead to miscommunication or misinterpretation by healthcare providers or insurance companies.
Here are some of the most frequent mistakes to watch out for:
- Lack of Clarity: Ensure that the purpose of the request is clear and easy to understand. Ambiguity can result in the document being overlooked or rejected.
- Insufficient Evidence: Failing to include relevant medical records, test results, or expert opinions can significantly reduce the credibility of the request.
- Omitting Key Details: Always include essential patient information, condition details, and a clear explanation of the treatment’s necessity. Missing information can delay the process.
- Overcomplicating the Language: Avoid using overly technical or complex terminology. The goal is to communicate effectively and clearly, ensuring the reader understands the medical justification.
- Ignoring Formatting: A poorly organized document may confuse the reader. Maintain a logical flow and use headings and bullet points to make the request easy to navigate.
How Healthcare Providers Assess the Request
When reviewing a treatment request, healthcare providers or insurers focus on the completeness and clarity of the submitted information. They evaluate how well the request justifies the need for the proposed intervention and whether it aligns with established medical guidelines. A thorough and well-organized submission increases the likelihood of a positive response.
Factors Healthcare Providers Consider
- Patient’s Condition: Providers assess the severity and specifics of the patient’s health issues. They need clear details on how the condition impacts the patient’s daily life and well-being.
- Proposed Treatment: Providers review the suggested course of action to ensure it is appropriate and aligns with accepted treatment protocols for the condition.
- Supporting Documentation: Relevant medical records, test results, and expert opinions are scrutinized to confirm the need for the recommended solution.
- Cost and Coverage: Insurers, in particular, evaluate whether the treatment is covered under the patient’s current plan and if it is deemed cost-effective.
What Makes a Strong Request?
- Clear Justification: A compelling case that explains why the suggested treatment is the most suitable option for the patient’s condition.
- Comprehensive Medical History: Including a complete history of the patient’s condition, treatments attempted, and responses is crucial for a solid evaluation.
- Detailed Explanation of Benefits: A strong request outlines how the proposed intervention will improve the patient’s health and quality of life.
Tips for Submitting Your Request
When submitting a request for treatment, the way you present your case can significantly affect the outcome. It is essential to ensure that all necessary documents are included, the format is clear and organized, and that all relevant information is readily available for the reviewer. A well-prepared submission can help avoid delays and improve the chances of approval.
Best Practices for a Successful Submission
| Tip | Description |
|---|---|
| Double-Check Documentation | Ensure that all necessary medical records, test results, and expert opinions are included. Missing documents can cause delays or result in the rejection of your request. |
| Follow Submission Guidelines | Adhere to the provider’s or insurer’s submission guidelines, including the format, required information, and any deadlines. This helps streamline the process and avoids complications. |
| Keep Copies of Everything | Make sure to keep copies of all the documents you submit. This way, you can refer to them if needed or provide additional information upon request. |
| Ensure Clarity and Precision | Present your case in a clear and organized manner. Use straightforward language to explain the medical justification and treatment need. |
| Follow Up | After submitting the request, follow up to confirm that all documents have been received and to inquire about the status of the review. |