Letter of Medical Necessity Template for Occupational Therapy
When seeking assistance with health-related services, a well-structured document plays a crucial role in communicating the need for specialized interventions. This document serves as a formal request from a healthcare provider, explaining why certain services are essential for the patient’s recovery or overall well-being. Such a request ensures that the necessary support is not only recognized but also properly processed by the relevant authorities or insurance companies.
The document typically outlines the patient’s condition, detailing how the recommended interventions will aid in improving their daily functions or address specific health challenges. By providing clear and precise information, the form facilitates understanding and encourages a positive response from the reviewing entity.
Having a comprehensive and professional approach to this request increases the likelihood of approval, ensuring the patient receives the care they require without unnecessary delays. Understanding the structure and content of such a request is key to its success, allowing healthcare providers to advocate effectively on behalf of their patients. In this section, we will explore how to create an effective and persuasive document that meets all the necessary criteria for a favorable outcome.
Understanding the Importance of Medical Necessity Letters
When seeking approval for essential health services, clear documentation is vital to ensure the patient receives the proper care. A structured request is an important step in demonstrating the need for specific interventions. It helps provide the necessary justification that supports the medical decision and outlines the expected benefits of the recommended treatments. Without this type of formal communication, it can be difficult for service providers or insurance companies to comprehend the urgency or value of the treatment.
Clarifying the Need for Support
Such a formal request outlines the patient’s condition and explains why a particular service is crucial for their recovery or well-being. It emphasizes how the proposed interventions will improve their quality of life and assist in daily tasks. This clarity is essential for the entity reviewing the case, enabling them to make an informed decision based on the detailed evidence provided.
Ensuring Timely Access to Care
Submitting a well-crafted request speeds up the process of obtaining approval. By presenting a clear, concise, and professional explanation, healthcare providers help facilitate timely access to necessary services. The more precise the information, the greater the chance of receiving a prompt response. This process helps avoid unnecessary delays and ensures the patient gets the care they need when they need it most.
How to Draft a Medical Necessity Letter
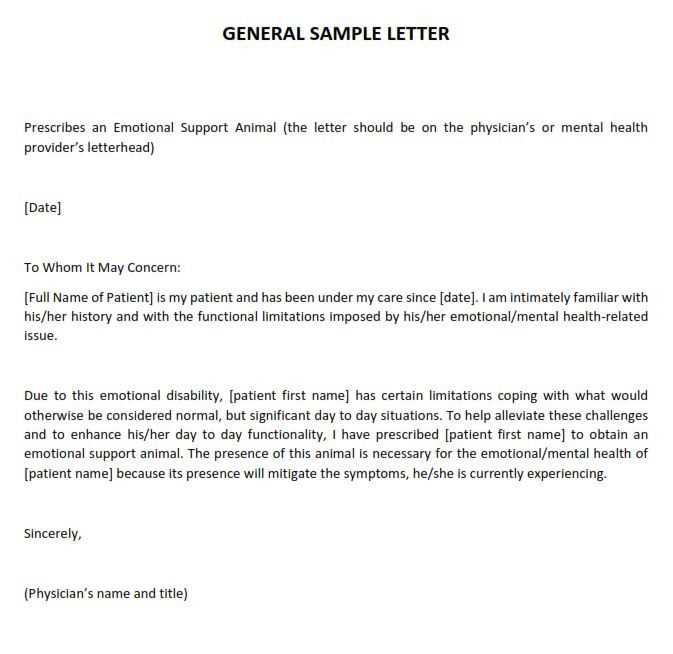
Creating a formal request for essential health services requires a careful approach to ensure that the need for specific care is clearly communicated. This document should be structured in a way that effectively explains the patient’s condition and the expected benefits of the proposed treatments. By doing so, it helps the reviewing entity understand why such interventions are vital for the patient’s well-being and recovery.
The first step in drafting this document is to begin with a brief introduction that clearly identifies the patient and their medical history. Following this, you should provide a detailed explanation of the current condition, highlighting any challenges the patient faces in daily activities. This section should emphasize the severity of the condition and the impact it has on the patient’s quality of life.
Next, outline the specific interventions being requested, explaining how they will address the patient’s needs. Be sure to include any relevant medical evidence or clinical findings that support the decision to pursue these treatments. The goal is to make it clear that the proposed care is not only appropriate but essential for improving the patient’s health outcomes.
Finally, conclude by summarizing the reasons why these interventions are necessary. Reaffirm the importance of timely access to the requested services and the positive outcomes expected from them. A well-structured request ensures that the reviewing body has all the information needed to make an informed decision and approve the requested support.
Key Components of an Effective Template
When drafting a formal request for specialized health services, certain elements are essential to ensure the document is comprehensive and compelling. A well-structured form should clearly communicate the patient’s needs, the supporting evidence for the proposed treatments, and the expected benefits. It should also be easy to follow and provide all necessary information in a concise yet thorough manner, allowing the reviewing entity to make an informed decision quickly.
One key component is the clear identification of the patient, including their medical history and relevant diagnoses. This section sets the stage by providing context and background, ensuring that the recipient understands the patient’s health condition before evaluating the need for services.
Another important element is a detailed description of the patient’s current condition, including any limitations they face and how these challenges affect their daily life. This section should highlight the severity of the situation, making it clear why the requested services are necessary for improving the patient’s well-being.
The request should also include specific details about the recommended services and how they will directly benefit the patient. Supporting documentation, such as clinical findings or expert recommendations, helps validate the necessity of the proposed interventions. Additionally, the document should outline the expected outcomes, showing how the services will improve the patient’s functional abilities and quality of life.
Finally, a well-organized closing statement reiterates the importance of timely access to the requested services and emphasizes how they are essential for the patient’s recovery or daily functioning. Including all these components ensures that the request is thorough, professional, and likely to be approved promptly.
Best Practices for Occupational Therapy Documentation
Effective documentation is a key aspect of ensuring that a patient receives the proper care and services. Properly recording a patient’s condition, progress, and the interventions being provided helps both the healthcare provider and the reviewing entity understand the necessity of certain treatments. Clear, detailed records also ensure that all relevant information is communicated accurately, promoting the best possible outcomes for the patient.
Here are some best practices for creating accurate and effective records:
- Be Clear and Concise: Use simple, straightforward language to explain the patient’s condition and the need for specific services. Avoid unnecessary jargon or overly complex explanations.
- Include Detailed Assessments: Provide a thorough evaluation of the patient’s current abilities, limitations, and challenges. This helps highlight the severity of their condition and justifies the request for interventions.
- Document Specific Interventions: Outline the exact services being recommended, along with their expected benefits. Be specific about how each intervention addresses the patient’s needs.
- Use Evidence-Based Information: Support your documentation with clinical evidence, expert opinions, or research that backs the decision to provide the recommended services.
- Track Progress Regularly: Document the patient’s progress over time, noting improvements or setbacks. This ongoing record helps assess the effectiveness of the interventions and informs future decisions.
- Ensure Proper Organization: Structure the documentation in a logical and easy-to-follow format. Use headings, bullet points, and clear sections to make the content more accessible.
By following these practices, healthcare providers can ensure that their documentation is comprehensive, clear, and effective in supporting the patient’s needs. Proper records not only streamline the approval process but also enhance the quality of care provided.
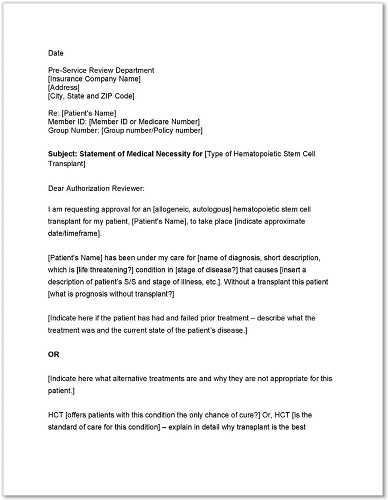
How to Submit Your Request to Insurers
Submitting a formal request to insurers is a crucial step in obtaining approval for necessary health services. To ensure a smooth process, it’s important to follow specific guidelines that help the reviewing entity quickly assess the document and make a timely decision. Understanding the requirements and proper submission methods can avoid unnecessary delays and improve the chances of approval.
First, verify the insurer’s submission guidelines. Many insurance providers have specific forms, portals, or methods through which requests must be submitted. Familiarizing yourself with these details will help ensure your submission complies with their expectations. Below is a table summarizing common submission methods and necessary details:
| Submission Method | Details |
|---|---|
| Submit the request as a PDF or scanned document attached to an email. Include any necessary reference numbers or patient information in the subject line. | |
| Online Portal | Upload the document through the insurer’s dedicated platform. Be sure to follow any prompts to ensure the correct form is submitted. |
| Fax | Send the completed request to the insurer’s designated fax number. Ensure all pages are clearly legible. |
| Postal Mail | Mail the request to the insurer’s office. Use certified mail if needed to confirm delivery and keep a copy for your records. |
After submission, it’s important to follow up. If the request is not processed within the expected time frame, contacting the insurer can help clarify any issues or provide additional information. Always keep copies of the request and any correspondence related to the submission to ensure proper documentation.
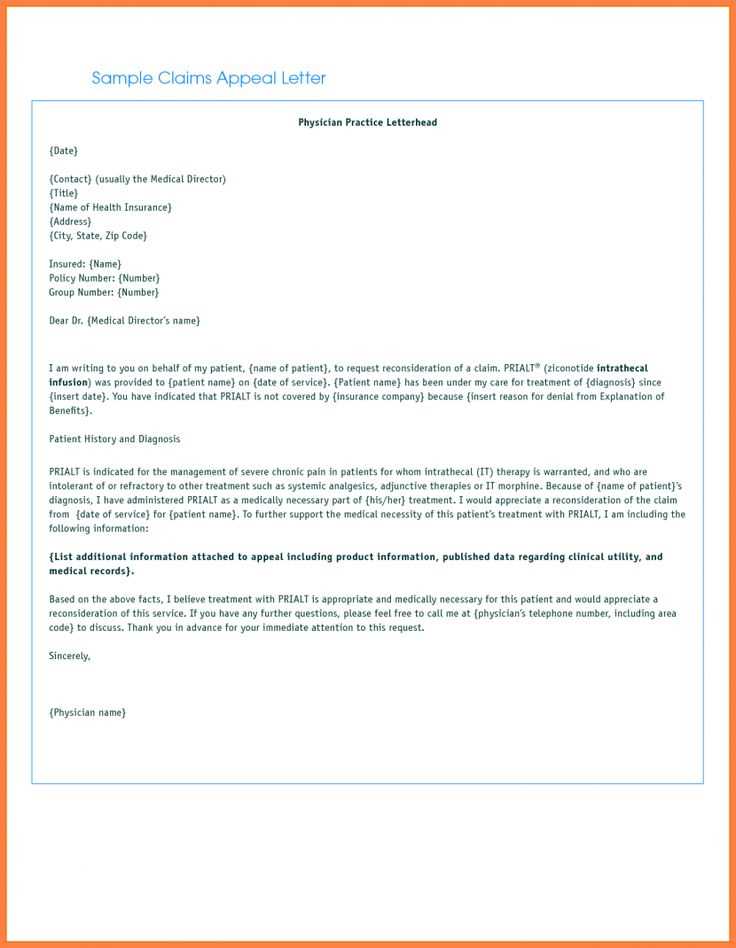
Common Mistakes to Avoid in Letters
When creating formal documents intended for insurers or healthcare providers, avoiding common errors is essential to ensure the submission is effective and processed efficiently. Many individuals unknowingly make mistakes that can delay or even derail their request. Understanding what to avoid can significantly improve the chances of approval.
One frequent mistake is the lack of sufficient supporting details. Failing to include clear evidence or comprehensive explanations regarding the patient’s condition and the proposed services can make it difficult for the recipient to evaluate the request properly. Ensure that each piece of information is relevant and well-documented.
Another issue is using vague or unclear language. It’s essential to avoid ambiguous phrases that don’t adequately describe the situation. Being specific about the patient’s condition and the need for treatment will provide a clearer understanding and stronger justification for the request.
Improper organization is also a common problem. If the document is difficult to read or navigate, it may confuse the reader, causing delays in the review process. Ensuring the document is well-structured, with distinct sections, headings, and bullet points, can make a significant difference.
Lastly, neglecting to follow submission guidelines can lead to the rejection of the request. Different insurers or healthcare providers have their own specific rules regarding documentation. Missing required information or submitting documents in the wrong format can lead to unnecessary complications.