Letter of medical necessity template
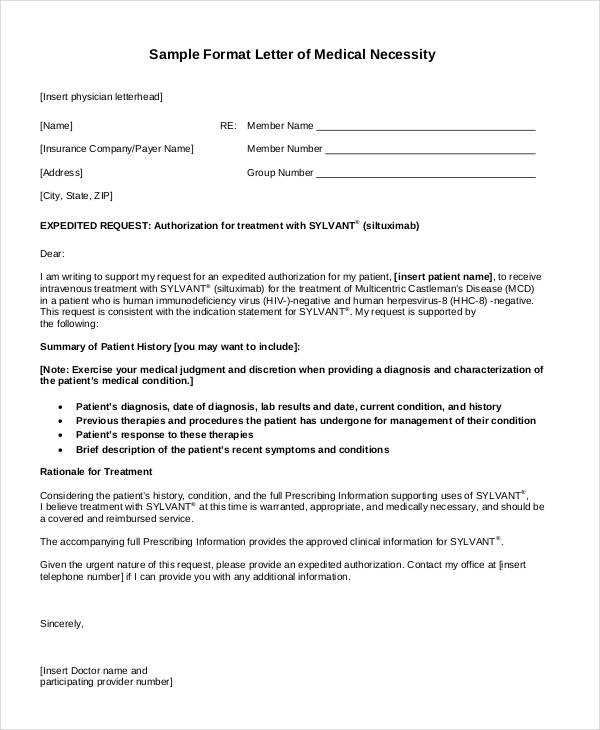
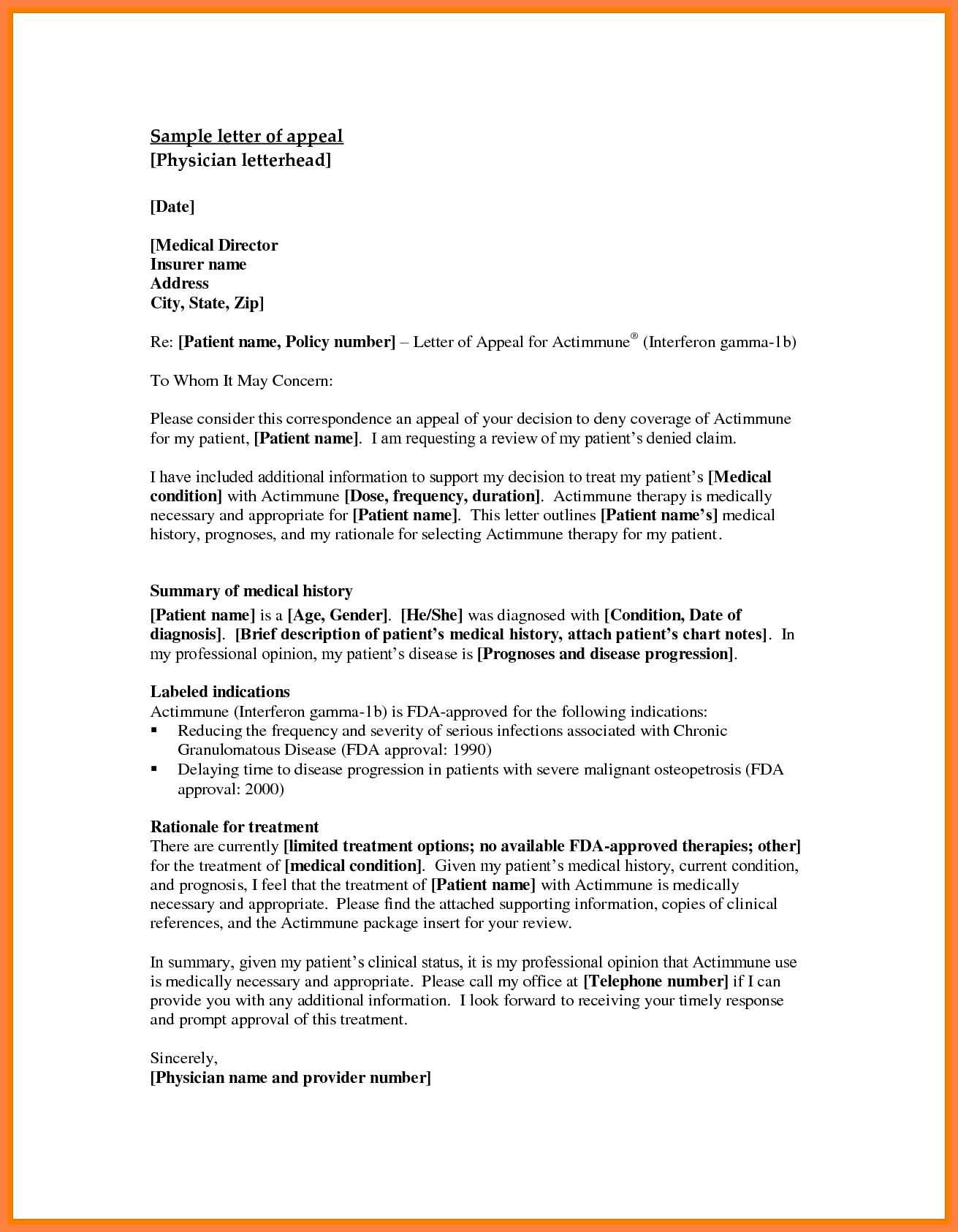
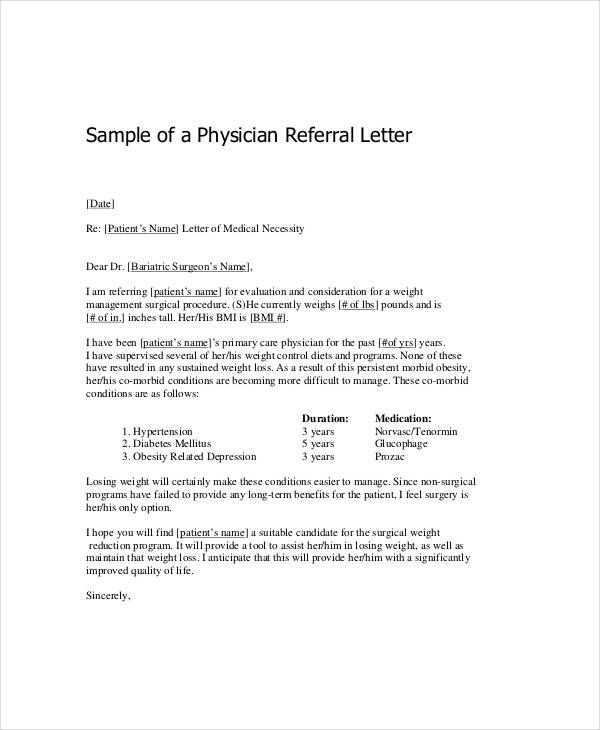
Begin the letter by clearly stating the purpose: to support a request for a medically necessary service or treatment. Specify the patient’s condition and the particular treatment, device, or service being requested. Ensure that the details are specific, including any relevant diagnosis codes or medical terms that validate the necessity of the request.
State the Medical Justification: Describe the patient’s condition and the medical reasoning behind the request. Include detailed information from medical assessments or doctor’s notes. Mention any tests, treatments, or medications that have been tried previously, and explain why the requested service or treatment is the most appropriate option at this point.
Be concise but thorough: Avoid long paragraphs or extraneous information. Focus on the key points that demonstrate why the treatment is required for the patient’s health and well-being. Mention how the service or equipment will directly benefit the patient’s recovery or quality of life.
Provide Supporting Evidence: Attach relevant medical documentation, such as lab results, imaging reports, or specialist recommendations, to back up the claim. This will strengthen the request and clarify why the service is not only necessary but urgent.
End with a clear request for approval, thanking the recipient for their time and consideration. Include your contact information in case follow-up is needed. Ensure the tone remains professional, direct, and respectful throughout the letter.
Here are the corrected lines based on your request:
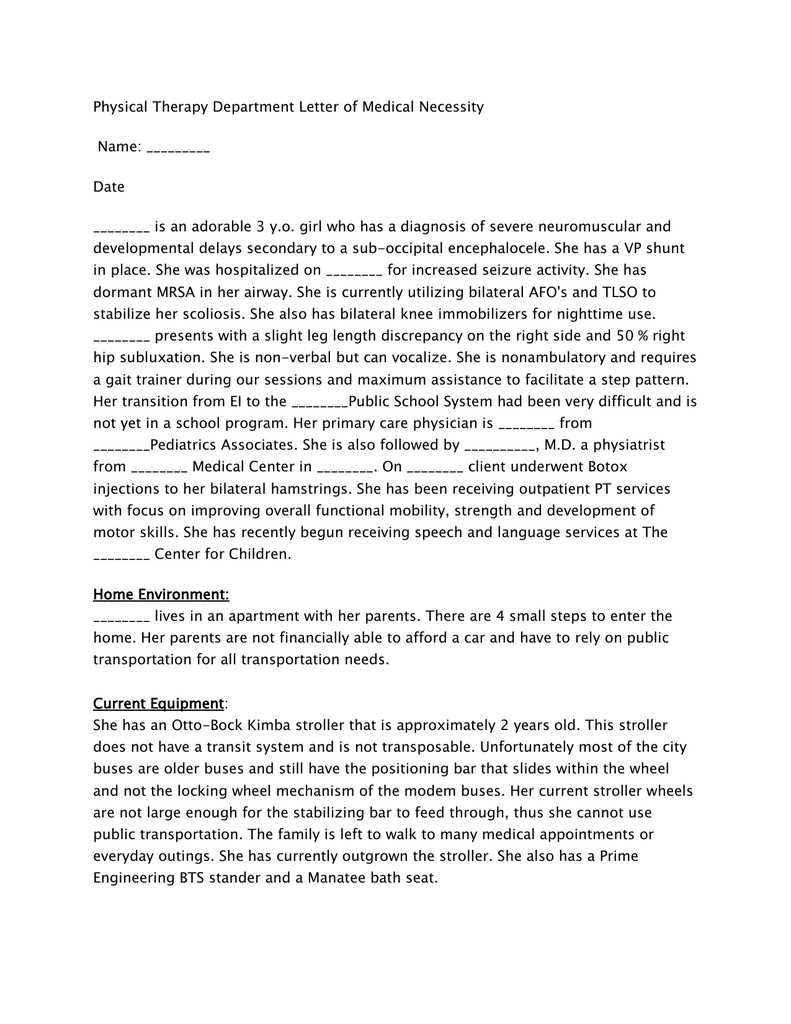
First, ensure that the medical necessity letter includes a clear statement from the healthcare provider explaining why the requested service or equipment is needed. This should be supported by specific clinical details.
Next, avoid vague or general language. Include specific diagnoses, treatment plans, and any relevant test results that demonstrate the need for the prescribed service or product.
Be sure to detail any previous treatments or therapies that have been ineffective, if applicable. This shows the progression and necessity of the requested service.
Lastly, include the duration of the treatment plan or required equipment usage. This helps establish the ongoing necessity of the request.
- Letter of Medical Necessity Template
The Letter of Medical Necessity (LMN) is a critical document required by insurance providers to justify the medical need for certain treatments, devices, or procedures. This letter helps ensure that coverage is approved for non-standard treatments or equipment. Below is a straightforward template to guide you in writing a Letter of Medical Necessity.
Make sure to include specific patient details, relevant medical history, and clear explanations of why the requested item or service is necessary for the patient’s treatment plan. Personalize this template according to the unique circumstances of each case.
| Field | Example |
|---|---|
| Patient Information | John Doe, DOB: 01/01/1980, Insurance ID: 123456789 |
| Physician Information | Dr. Jane Smith, MD, Address: 123 Medical St., City, State, ZIP, Phone: (123) 456-7890 |
| Diagnosis | Chronic Knee Pain, ICD-10 Code: M17.0 |
| Requested Item or Service | Prescription for Custom Knee Brace |
| Medical Necessity Justification | The patient suffers from chronic knee pain due to osteoarthritis. The prescribed custom knee brace will alleviate discomfort and prevent further joint damage, enhancing mobility and quality of life. Conservative treatments, such as physical therapy and pain medications, have been ineffective in managing symptoms. |
| Additional Information | The knee brace has been recommended by the patient’s orthopedic specialist as part of the ongoing treatment plan. |
Ensure to attach any supporting documents, such as medical records or previous treatment details, to substantiate the request. The letter should be signed and dated by the prescribing physician.
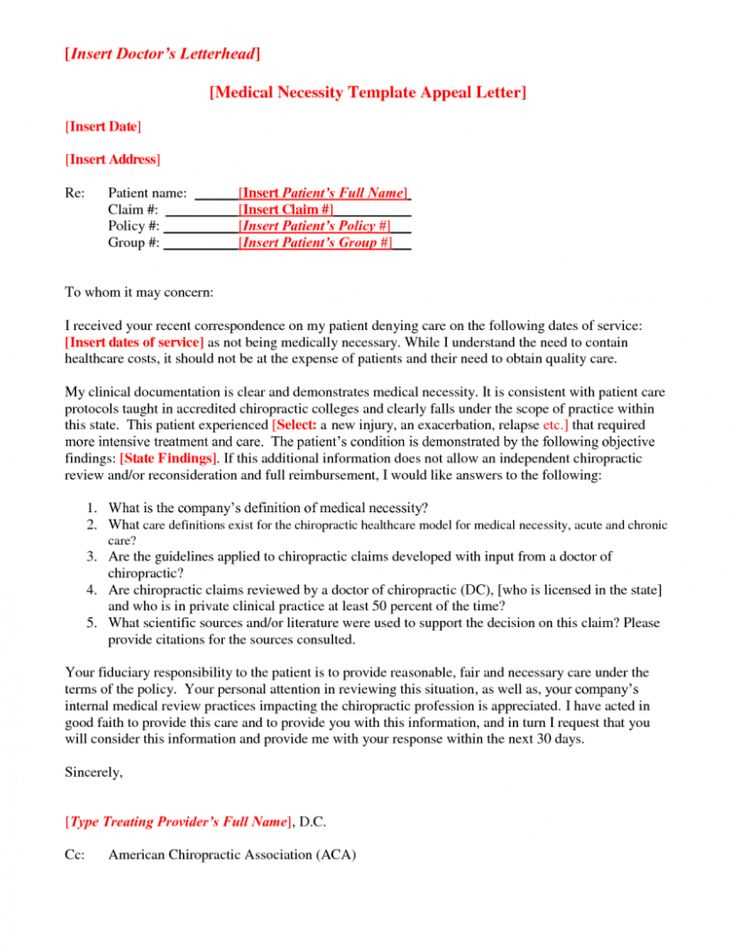
Begin with a clear, concise heading that identifies the purpose of the letter, such as “Request for Insurance Approval.” Follow with the recipient’s name, position, and company. If the recipient is unknown, simply address the letter to “To Whom It May Concern.”
Next, introduce the purpose of the letter in the opening paragraph. State your request directly, specifying the treatment, service, or equipment that needs approval. Mention the patient’s name, insurance policy number, and any relevant dates for clarity.
The body should provide supporting details that justify the request. Include medical diagnosis codes, supporting physician recommendations, and any relevant test results. Be sure to highlight how the treatment or service aligns with the patient’s medical needs and well-being.
Close the letter by requesting a timely response. Express appreciation for their consideration and offer to provide additional information if necessary. Include contact details for follow-up.
End with a formal sign-off such as “Sincerely” followed by your name and title. If applicable, include a signature for added professionalism.
A well-structured medical necessity letter must clearly outline the justification for specific treatments. Each treatment should be addressed with attention to relevant clinical details and supporting evidence.
1. Treatment Description and Rationale
Provide a precise description of the treatment being requested, including the method, duration, and expected outcome. State why this particular treatment is the most appropriate choice for the patient’s condition based on clinical guidelines and research evidence.
2. Diagnosis and Medical History
Detail the patient’s diagnosis, including any relevant medical history that supports the need for the treatment. Reference specific tests, symptoms, or conditions that make the proposed treatment a necessary option.
3. Previous Treatment Attempts
Include a summary of past treatments and their outcomes. Highlight any unsuccessful attempts or adverse reactions to other therapies that demonstrate the necessity of the requested treatment.
4. Expected Benefits
Outline the anticipated improvements in the patient’s health or quality of life. Use medical evidence, such as studies or expert opinions, to demonstrate how the treatment will address the patient’s needs.
5. Impact of Delay
Explain the consequences of delaying or denying the requested treatment. Include potential risks or the progression of the patient’s condition if the treatment is not administered in a timely manner.
6. Clinical Guidelines or Expert Recommendations
Reference clinical guidelines, peer-reviewed studies, or recommendations from recognized medical experts to strengthen the argument for the treatment’s necessity. These resources provide credibility and reinforce the legitimacy of the request.
Use clear, direct language to outline the medical necessity of the treatment or service. Start by specifying the condition and how the requested treatment addresses it. Focus on the connection between the diagnosis and the recommended intervention.
Highlight how the treatment will improve the patient’s health outcomes, using precise medical terminology that aligns with the healthcare provider’s expertise. Use phrases like “clinically proven,” “evidence-based,” and “recommended for this condition” to show the relevance of the request.
Reference current guidelines or expert consensus supporting the treatment. Terms like “standard of care,” “peer-reviewed studies,” and “leading medical research” establish credibility. Incorporate data-driven language, such as “studies show,” “demonstrated benefits,” or “recommended dosage,” to strengthen the argument.
Be concise but include all critical facts. Emphasize any immediate or long-term benefits, such as reduced hospitalization or improved quality of life. State any previous attempts at treatment and explain why alternative options have not been effective, using terms like “ineffective,” “suboptimal response,” or “unsuccessful trial.”
Keep the tone respectful and professional, avoiding unnecessary emotional appeals. Use terminology that aligns with the healthcare provider’s perspective, demonstrating that the request is grounded in solid clinical reasoning.
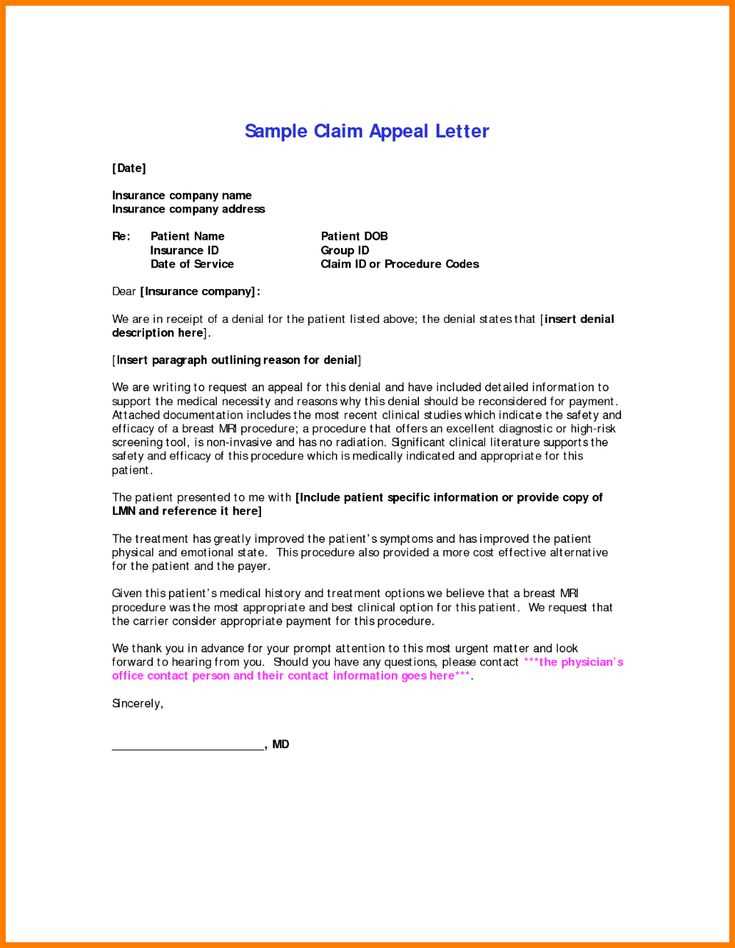
Begin by collecting all relevant medical records, including diagnosis, treatment history, and any previous tests or procedures related to the condition. Ensure you have the most recent documentation from healthcare providers that outlines the severity of the condition and how the requested treatment or service will improve health outcomes.
Obtain letters from specialists or attending physicians explaining why the requested treatment is necessary. These letters should address specific aspects of the medical condition and outline how the proposed service will directly address the patient’s needs. Include any test results or diagnostic images that support the need for the treatment.
If applicable, include any prior authorization requests or claims for similar treatments that have been denied. Providing this information helps demonstrate the necessity for approval and can clarify why the new request should be considered differently. Include any notes from consultations or second opinions that back up the case for medical necessity.
Gather documentation that may demonstrate the failure of previous treatments or interventions. This could include therapy notes, progress reports, or results from prior surgeries or medications that were ineffective. Make sure all documentation is up-to-date and clearly demonstrates the need for the requested service.
Common Mistakes to Avoid When Writing a Letter for Medical Necessity
Focus on the key facts and avoid vague statements. Be clear and specific when describing the patient’s condition and why the requested treatment is necessary. Avoid general terms that do not directly relate to the patient’s needs.
1. Lack of Detailed Medical Justification
Avoid providing insufficient medical explanation for the treatment. Instead, clearly explain how the requested treatment aligns with the patient’s medical condition. Include relevant clinical evidence, such as test results or medical history, to support your case.
2. Using Unclear or Jargon-Filled Language
Ensure the letter is written in a straightforward manner. Avoid medical jargon that may confuse the reader, especially if they are not familiar with the specifics of the patient’s condition. Aim for clarity and precision with each term used.
3. Failing to Address Insurance Policy Requirements
Review the insurance company’s guidelines before drafting the letter. Ensure the content aligns with the criteria they expect, such as the necessity of the treatment and the patient’s failure with previous treatments. Ignoring these requirements could result in denial.
4. Not Providing Enough Documentation
Without adequate documentation, the letter may not hold sufficient weight. Attach any relevant medical records, such as lab results, imaging studies, or referral notes that support the necessity of the proposed treatment.
5. Neglecting to Use Professional Tone
Avoid being overly casual or overly emotional in the letter. Maintain professionalism throughout, ensuring the focus remains on the medical facts and the need for the treatment.
6. Overlooking the Timeliness of the Request
Don’t wait until the last minute to submit the letter. Ensure the letter is sent well in advance to allow for adequate processing time, especially if the treatment is urgent or time-sensitive.
How to Tailor Your Letter for Different Insurance Plans
Address specific requirements of each insurance plan to maximize approval chances. Review the plan’s coverage guidelines and mention relevant details clearly. For instance, some insurers prioritize detailed medical justification, while others focus more on cost comparisons. Adapt your language to match the insurer’s preferences to avoid delays.
1. Understand Coverage Criteria
Study the insurer’s policy before writing. Identify covered services, exclusions, and specific documentation requests. For example, if an insurance provider requires extensive medical history, ensure your letter includes relevant treatments, diagnoses, and any prior approvals. This approach helps meet insurer expectations and streamlines the review process.
2. Use Precise Terminology
Different insurers may use different terminology. Ensure your letter uses the same medical terms, treatment names, and coverage language the insurance company uses. If the insurer uses specific codes or abbreviations, incorporate them to align with their documentation style. This reduces the risk of your letter being flagged for incorrect or missing information.
Tailoring your letter increases its effectiveness and can shorten approval times. Each plan has unique priorities, so aligning your approach to these can make all the difference in the outcome.
Start by making sure the letter is addressed to the right recipient, such as the insurance company or healthcare provider. Use the correct name and title of the person in charge to ensure accuracy.
Clearly state the medical condition and why specific treatment or equipment is needed. Provide relevant details that can help explain the necessity, such as the diagnosis, symptoms, and how the prescribed treatment will alleviate them.
Support your request with any available medical records, test results, or previous treatments. Including these documents strengthens the case and shows the severity of the condition.
Ensure the letter is concise, but detailed enough to provide all necessary information. Avoid unnecessary medical jargon; instead, focus on explaining the situation in a way that is understandable to someone who may not be familiar with the specifics of the condition.
Conclude by requesting approval for the specific treatment or equipment and mention the urgency of the matter if applicable. Close the letter with a polite statement, such as offering to provide further information if needed.