Medical billing appeal letter template
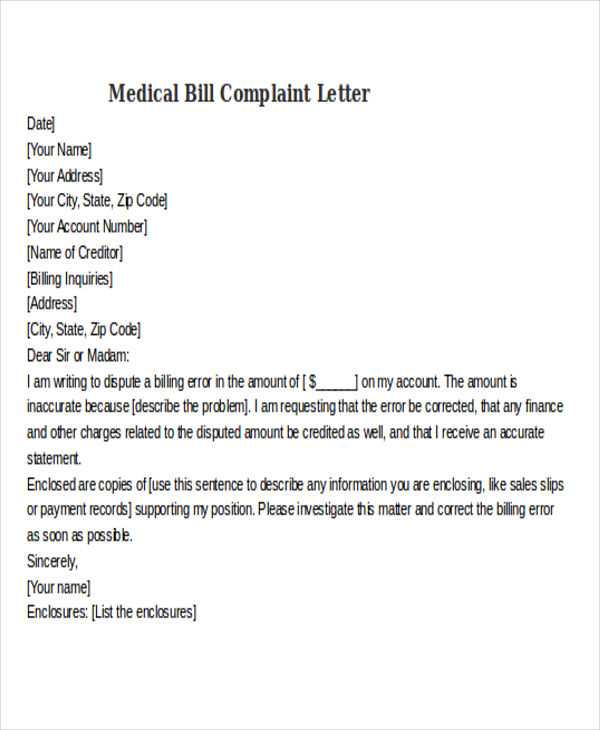
Write a clear and direct appeal letter when disputing a medical billing issue. Start by referencing the date of service and the specific charges in question. Use factual details to explain why you believe the billing is incorrect or why you think the insurance should cover more of the cost. Be polite but firm in your tone, ensuring all relevant information is included.
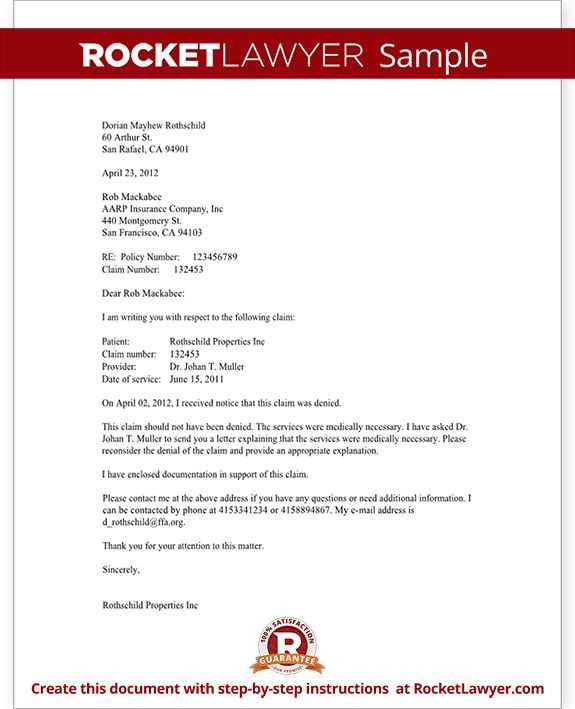
Address the letter to the billing department, using the contact details provided on your statement or insurance card. Include your account number, the patient’s name, and any claim numbers associated with the dispute. If the issue involves insurance denial, refer to the specific denial code and clarify why the claim should be reconsidered.
Clearly state what action you are requesting, whether it’s a reevaluation of the charges, full or partial payment, or a correction of any billing errors. Attach any supporting documentation, such as medical records, test results, or correspondence with your insurance company. This helps to strengthen your case and makes it easier for the billing department to understand your position.
Finish by expressing your expectation for a timely resolution. Include your contact information and request that they respond within a specific time frame. A courteous but assertive approach increases the likelihood of a positive outcome.
Here’s a detailed plan for an article titled “Medical Billing Appeal Letter Template” in HTML format, with 6 specific, practical headings:
1. Introduction to Medical Billing Appeals
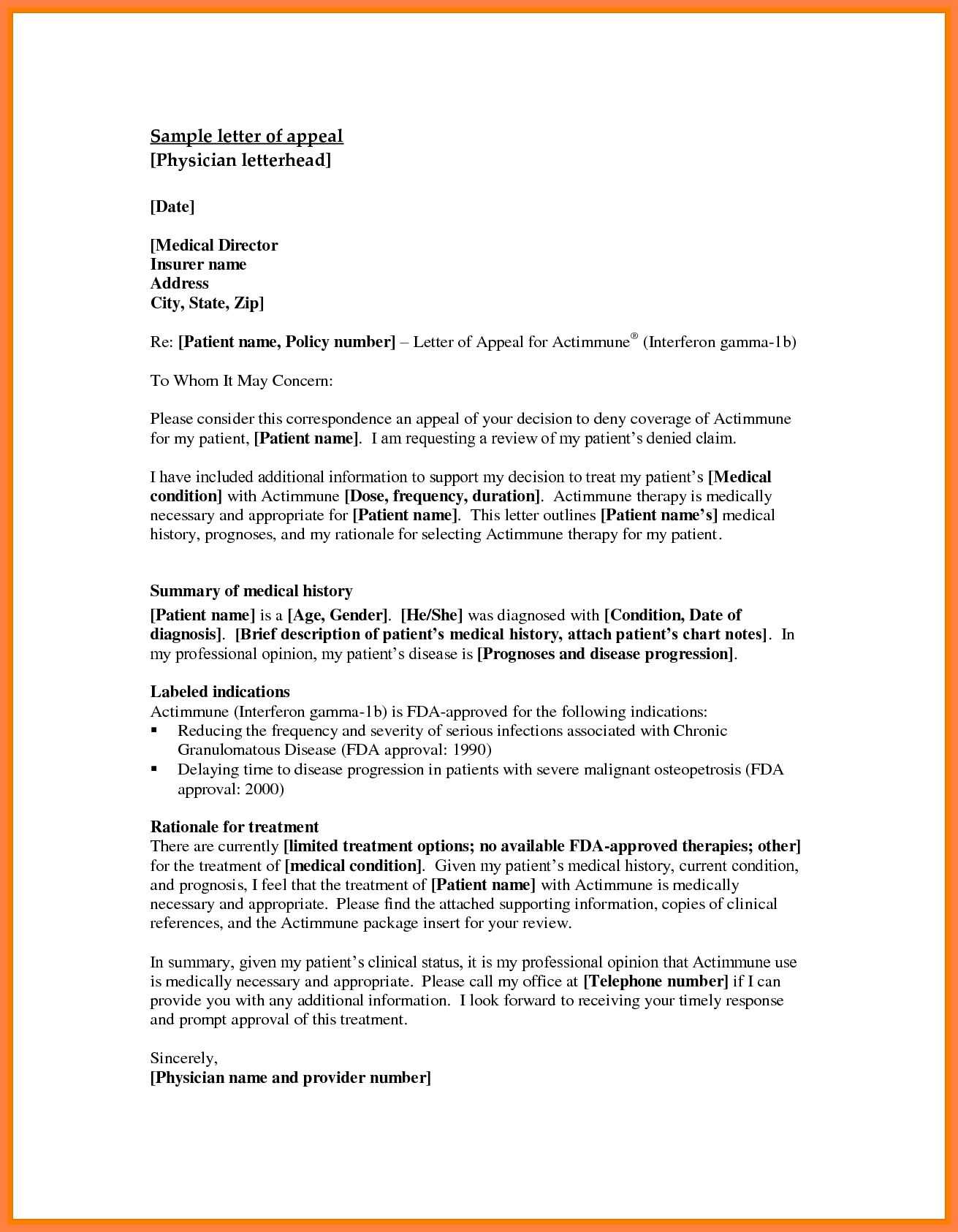
Start by explaining the purpose of a medical billing appeal letter. This is a formal request to a health insurance company to review and possibly overturn a denied claim. Be specific about why understanding how to write an appeal letter is crucial for both patients and healthcare providers.
2. Key Elements of an Appeal Letter
Detail the components that must be included in an appeal letter. Mention the patient’s personal information, account number, a clear explanation of the denial reason, and supporting evidence or documentation. Highlight the importance of being clear and concise, avoiding unnecessary jargon.
3. How to Address the Insurance Company
Provide tips on how to properly address the insurance company in the letter. Include the correct format for the recipient’s details, such as the department and contact person. Emphasize the need to use polite and professional language to ensure a constructive response.
4. Crafting a Strong Argument for the Appeal
Guide readers on how to build a strong case for why the claim should be reconsidered. Mention reviewing the original bill, understanding policy coverage, and comparing the service against the insurance policy. Suggest including any discrepancies or errors found in the original billing process.
5. How to Include Supporting Documentation
Explain the types of supporting documents that should accompany the appeal letter, such as medical records, receipts, or previous correspondence with the insurance company. Advise organizing documents in a clear order to strengthen the case.
6. Closing and Following Up
Conclude the appeal letter by summarizing the request and expressing a desire for prompt reconsideration. Stress the importance of including contact information for follow-up. Include a note about following up regularly to ensure the appeal is being processed in a timely manner.
- How to Address the Insurance Company
Begin with a clear and formal greeting. Use the name of the representative if known, or simply “Dear Claims Department” if you’re unsure. Ensure the tone remains professional and respectful throughout. Include the claim number or reference number at the beginning of your letter for easy identification.
Example: “Dear Claims Department, Reference: Claim #123456789”
Address the letter to the correct department or individual. If you’re sending the letter to an email address, verify the contact details before proceeding to avoid delays. If you’re sending a physical letter, ensure that the address is accurate and complete, including any specific department or office that handles billing appeals.
Be specific about the nature of your request. If possible, mention the reason for your appeal in the first paragraph to give immediate context to your letter.
Include the patient’s full name, account number, and the specific dates of service for the claim in question. This helps the reviewer quickly identify the correct case and prevents confusion with other claims. Clearly state the reason for your appeal. Be precise, and provide any supporting evidence or documents that back your claim, such as medical records, test results, or relevant notes from healthcare providers.
Details of the Denial
Summarize the reason provided for the denial. Reference the specific codes or terms used by the insurance company. This gives clarity to both parties about what needs to be reconsidered. If the denial is based on missing information, ensure all relevant details are included in your appeal.
Justification for the Appeal
Provide a clear argument explaining why the claim should be reconsidered. Point out any errors in the initial assessment or highlight misinterpretations of policy terms. If the treatment was medically necessary, explain why and how it aligns with the insurance plan. Attach any additional documentation that supports your argument.
Lastly, include your contact information and a request for further clarification if needed. Be sure to keep the tone polite but firm. This helps establish your credibility and ensures that the appeal is taken seriously.
Review each bill carefully to identify discrepancies in charges or services provided. Compare the billed items against medical records and the explanation of benefits (EOB) provided by your insurance company.
- Check for Duplicate Charges: Ensure that the same procedure or service is not billed multiple times. Look for identical codes or descriptions for the same date of service.
- Verify Procedure Codes: Ensure that the correct medical codes (CPT, ICD-10) are used. If there’s a mismatch between the services rendered and the codes, request a correction.
- Examine Service Dates: Confirm that the dates of service match what you received. Sometimes, clerical errors can lead to incorrect dates being billed.
- Confirm Insurance Coverage: Double-check that the services billed are covered under your current policy. If a service should be covered but isn’t, contact your insurer for clarification.
- Review Discounts or Payment Adjustments: Ensure that any discounts, co-payments, or deductibles have been applied correctly based on your plan.
If you identify an error, contact the billing department immediately. Provide clear documentation, such as medical records, EOBs, and any correspondence with your insurance company. Request an itemized statement if one was not initially provided to help with clarity.
- Submit a Formal Appeal: If the error isn’t resolved through a simple inquiry, file a formal appeal. Include all relevant documentation and state the correction you seek.
- Follow Up Regularly: Keep track of your communication with the billing department or insurance company. If there is no response within a reasonable time frame, follow up to ensure the issue is being addressed.
Begin by clearly referencing the exact billing codes used in the original claim. Use the format provided by the insurer, typically either ICD, CPT, or HCPCS codes. Ensure accuracy when listing the code numbers to avoid confusion or rejection of the appeal.
Locate the Codes in the Claim Documentation
Identify the specific codes associated with the disputed charges. Refer to the Explanation of Benefits (EOB) statement or the original claim form. Ensure you are citing the correct version of the code, as sometimes updates or revisions may impact coding accuracy.
Provide Supporting Documentation
For each code you reference, attach supporting documentation. This can include medical records, test results, or notes from healthcare providers that validate the use of the cited codes. The more clear and concise your evidence, the more likely your appeal will succeed.
Double-check for any possible coding errors before submitting the appeal. Mismatched codes or missing information can result in further delays or denials.
Ensure all documents are clear, accurate, and complete. Ambiguity can lead to delays or denials. Focus on providing precise details that align with the services rendered and the treatment provided.
1. Include Detailed Itemization
- Provide a full breakdown of services, including dates of service and CPT/ICD-10 codes where applicable.
- Include descriptions of the procedures and treatments, matching them with the patient’s diagnosis to establish a clear connection between treatment and medical necessity.
2. Provide Legible and Signed Forms
- Ensure that all forms, including medical records and physician notes, are legible and signed by the appropriate healthcare provider.
- Check that signatures are up-to-date and consistent across all forms, especially for authorizations and consents.
3. Submit Relevant Medical Records
- Attach medical records that directly support the appeal. These can include progress notes, lab results, diagnostic imaging reports, and consultation notes.
- Only include relevant documents that directly relate to the disputed claim to avoid overwhelming the reviewer with unnecessary paperwork.
4. Avoid Generic Statements
- Provide specific and detailed explanations instead of general statements. For example, instead of saying “procedure was medically necessary,” describe the condition, symptoms, and why the treatment was required.
5. Double-Check Insurance Guidelines
- Review the payer’s specific documentation requirements and submit the exact information they request. This reduces back-and-forth and ensures that your appeal is processed efficiently.
Focus on being clear and concise. Avoid writing long, confusing sentences that can make it difficult for the reviewer to understand your case. Stick to the facts and keep the appeal as straightforward as possible.
1. Failing to Provide Complete Documentation
Ensure that all necessary documents are included in the appeal. Missing paperwork, such as medical records or proof of services rendered, can delay or even result in the denial of your claim. Double-check all required attachments before submitting.
2. Using Vague Language
Be specific about what you are appealing and why. Vague terms like “I disagree” or “this seems unfair” don’t provide enough information for the payer to assess the situation properly. Instead, clearly explain the reason for the dispute and back it up with concrete evidence.
3. Ignoring Appeal Deadlines
Submit your appeal on time. Each payer has specific deadlines for submitting an appeal. Missing these deadlines can result in an automatic denial. Check the time frame outlined in the initial denial notice and be sure to meet it.
4. Not Understanding the Reason for Denial
Before writing the appeal, fully understand why the claim was denied. A lack of clarity on the reason for the denial can lead to irrelevant or incorrect responses in the appeal. Review the denial notice carefully and address the specific issue raised.
5. Being Too Emotional
Keep the tone professional. Emotional language or personal feelings rarely help the situation and may even work against you. Stick to objective facts, and avoid using phrases that might be seen as unprofessional or confrontational.
6. Repeating the Same Information
Don’t repeat information that’s already been submitted. Restating the same facts without adding new or relevant details can make your appeal appear less thoughtful and waste the reviewer’s time. Provide new insights or explanations to strengthen your case.
7. Using Unclear Formatting
Make your appeal easy to read and understand. Use bullet points or numbered lists to break down complex information. Avoid large blocks of text and ensure that your appeal is organized logically.
Ensure the appeal letter is clear and to the point, addressing the specific issue at hand. Begin by referencing the claim number and the reason for the appeal. Highlight the particular charges that were denied or reduced and provide details on why these charges are valid. Use accurate billing codes and dates of service to support your claim.
Provide any supporting documents such as medical records, treatment plans, or physician’s notes that reinforce the validity of the services provided. If applicable, include expert opinions or additional documentation that clarifies any misunderstandings.
Always address the letter to the right person or department handling your claim. Ensure the tone remains professional, while clearly stating the desired outcome–whether it’s the reversal of a denial, a reconsideration of the billed amount, or the clarification of a misinterpretation of the services rendered.
| Information | Details |
|---|---|
| Claim Number | [Claim Number] |
| Patient Name | [Patient Name] |
| Service Date | [Date of Service] |
| Denial Reason | [Reason for Denial] |
| Appeal Request | [Desired Outcome] |
Be sure to follow the insurer’s specific appeal process and include any forms or references required. A well-documented, concise appeal can significantly improve the chances of a favorable outcome.