Cobra Open Enrollment Letter Template for Employers
Effective communication of health plan options is crucial for employees to make informed decisions regarding their coverage. A well-crafted document ensures that individuals fully understand their rights and available benefits, allowing them to choose the best plan for their needs.
Providing clear instructions and necessary details is vital for preventing confusion and errors during the process. By using an organized structure, employers can help employees navigate through the benefits selection period smoothly, ensuring compliance and satisfaction on both sides.
Whether you are creating an informative guide or a formal notification, the key is to present the information in a simple, direct manner. Properly conveying these details can significantly impact employee engagement and understanding of the benefits available to them.
What is a Health Benefits Notification
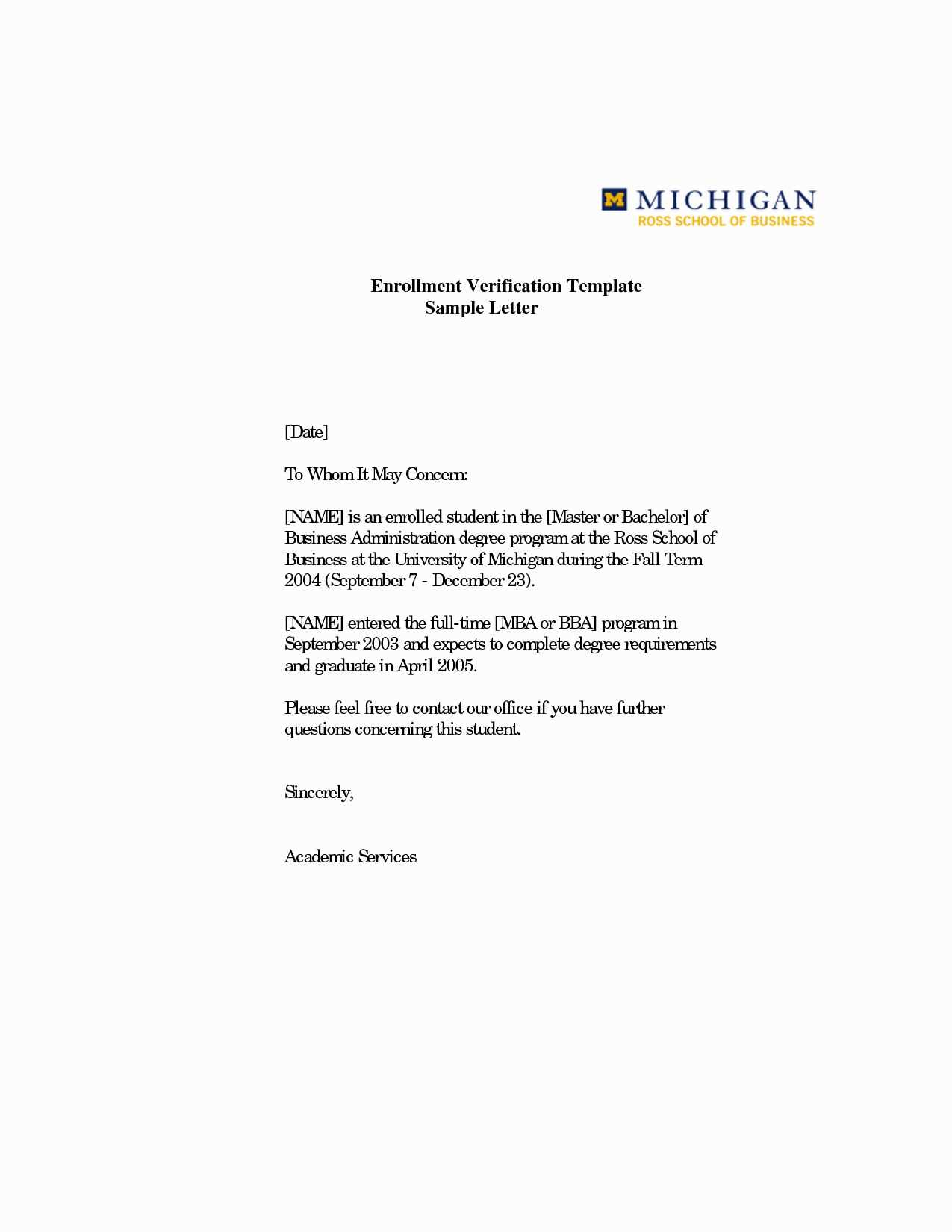
A health benefits notification is a formal communication from an employer to their employees, informing them about upcoming opportunities to review and adjust their health coverage. It serves as a reminder that employees should take action if they wish to continue, change, or select their benefits for the upcoming period.
The document typically provides detailed instructions on how to access available plans, deadlines for decision-making, and any required actions for continued coverage. This is an essential part of managing employee health options and ensuring they are aware of their entitlements and responsibilities.
In some cases, it may also include information about the continuation of benefits after certain life events, offering employees the chance to maintain coverage even after their employment status changes. This helps ensure that individuals do not lose access to vital health services during transitions.
Importance of Clear Communication for Employees
Clear communication is essential when conveying important information about benefits to employees. Providing detailed and understandable instructions ensures that individuals fully grasp the choices available to them, which helps them make informed decisions regarding their coverage options.
Without clarity, employees may struggle to understand their entitlements, leading to confusion, missed deadlines, or even incorrect selections. This can result in unnecessary stress and dissatisfaction, both for employees and employers.
By using precise language and organizing the information effectively, employers can promote transparency and trust. A well-structured communication strategy empowers employees to take the necessary steps for securing the best health benefits for themselves and their families.
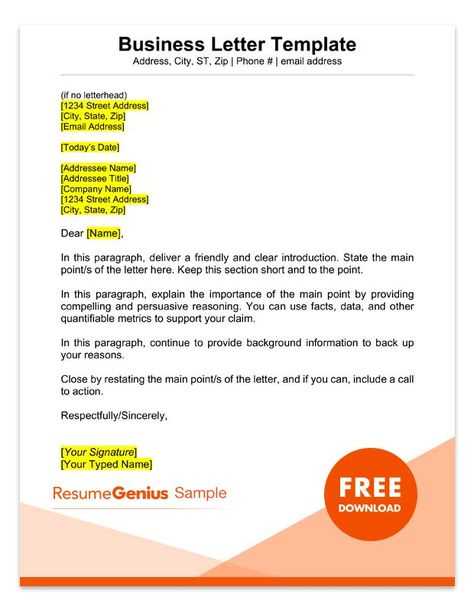
How to Create a Benefits Notification
Creating a benefits notification requires careful attention to detail and a clear structure to ensure employees understand the necessary actions they must take. The document should begin with a concise introduction, outlining the purpose and importance of the communication.
Next, include specific instructions on how employees can review and select their coverage options. Provide all relevant dates and deadlines to ensure no one misses crucial steps in the process. It’s also helpful to explain any changes to benefits or new plans that may be available for the upcoming period.
Lastly, ensure the letter is easy to navigate by using bullet points or lists, highlighting key information. This helps employees find the details they need quickly and efficiently, reducing the risk of confusion or mistakes.
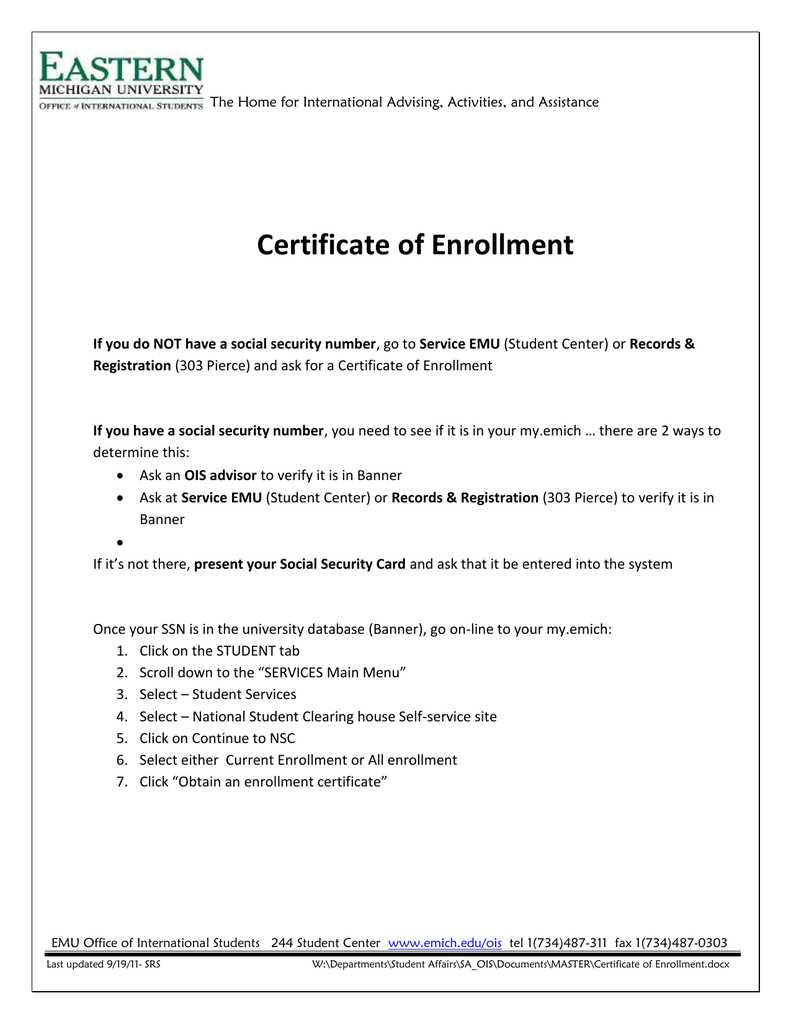
Key Elements to Include in the Notification
When crafting a benefits notification, it’s essential to incorporate several critical elements to ensure the message is both informative and actionable for employees. Start by clearly stating the purpose of the communication, emphasizing the importance of reviewing and selecting coverage options.
Next, include specific instructions on how employees can make their selections or changes. Provide clear steps for accessing benefits information, whether through an online portal or by contacting HR. It is also crucial to outline deadlines so employees are aware of the time frame to complete their decisions.
Additionally, include details about any changes in the benefits offerings, such as new plans, coverage modifications, or pricing adjustments. This helps employees make informed choices. Finally, contact information for further inquiries should be provided to ensure employees can easily reach out if they need assistance.
Common Mistakes to Avoid in Benefits Notifications
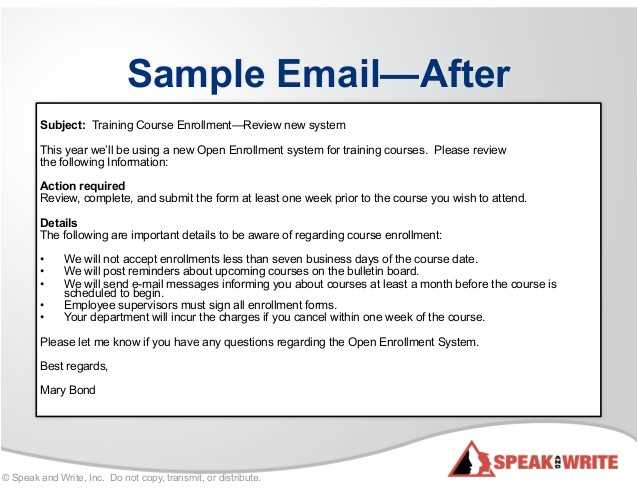
When preparing a benefits notification, several common errors can diminish its effectiveness and lead to confusion. Avoiding these mistakes ensures that employees receive clear, actionable information, which ultimately helps them make informed decisions about their coverage.
- Vague Language: Using unclear or complex language can confuse employees. Always strive for simplicity and clarity, making it easy for employees to understand their options and the necessary steps.
- Missing Deadlines: Not clearly stating the important deadlines can result in employees missing their chance to make decisions. Be specific about dates and ensure they are highlighted in the notification.
- Lack of Contact Information: Failing to include clear contact details for further questions can leave employees uncertain about where to seek help. Always provide a point of contact, such as HR or a benefits coordinator.
- Omitting Key Plan Details: Not mentioning critical updates or changes to the available plans can cause employees to overlook important adjustments. Always include information on any new offerings or changes to existing coverage.
By avoiding these mistakes, you can ensure that your communication is efficient and that employees are well-informed throughout the process.