Coordination of Benefits Letter Template for Patients
In the world of healthcare and insurance, clear communication is essential to avoid confusion and ensure timely payments. One key document that plays a role in this process is the formal notification provided to individuals when multiple insurance providers are involved in covering a claim. This document helps clarify the responsibilities of each provider and outlines the next steps for all parties involved.
Accurate and well-structured notifications are crucial for patients and insurance companies alike. By detailing the specifics of coverage and payment, it ensures there is no misunderstanding regarding who is responsible for what. Without such clarity, delays and errors in billing are common, which can lead to unnecessary complications for individuals seeking care.
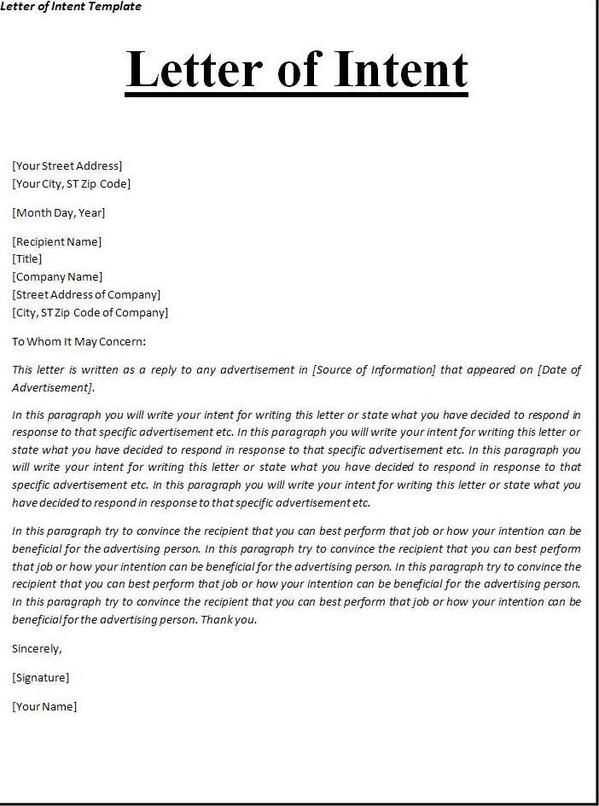
Crafting a professional and precise notification requires attention to detail. Each piece of information must be carefully included to make sure both the insured and the provider understand the exact terms. By following a standard format, individuals can streamline the entire process, making it easier to manage claims efficiently.
Purpose of the Benefits Notification
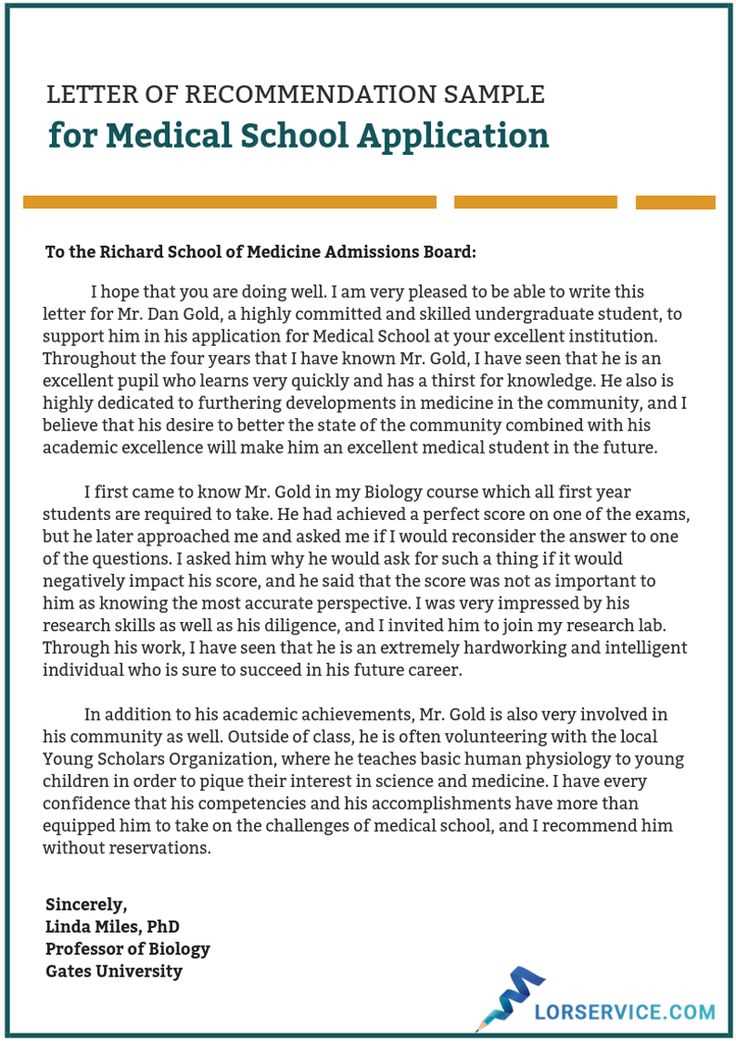
One of the primary objectives of this document is to ensure transparency between individuals and insurance providers when multiple policies are involved. It serves as a clear communication tool that outlines the financial responsibilities of each insurer and informs the recipient about the steps they need to take to resolve any outstanding issues. By providing essential information in a concise format, it helps avoid confusion and potential delays in coverage processing.
This notification helps eliminate uncertainties regarding which party will pay for specific healthcare expenses. It outlines the order of payment, indicating which insurance provider is responsible for what portion of the cost. Without such clarification, patients might be unsure of how their claims are being handled, leading to delays or misunderstandings about what will be covered.
By keeping all parties informed, the document facilitates smoother communication between the insured and their healthcare providers. When everyone is on the same page about insurance coverage, it reduces the chances of claims being rejected or disputed. This clarity ensures that individuals can focus on their health care without unnecessary administrative stress.
How to Create a Benefits Notification
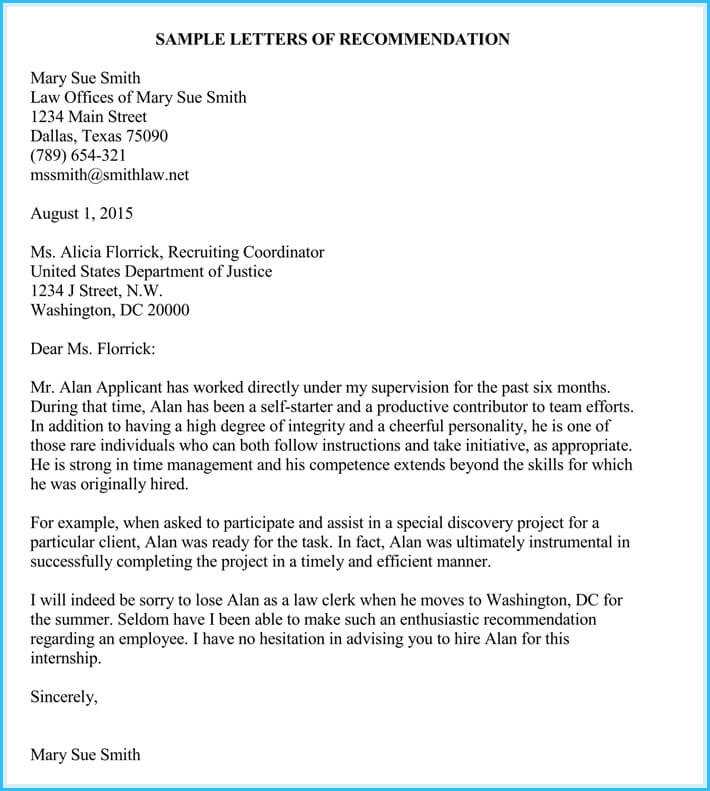
Designing a clear and effective communication document requires careful attention to the needs of both the recipient and the insurance providers. This document should clearly outline the key details of the coverage and the steps required from all parties involved. The goal is to ensure that the individual understands the financial aspects of their healthcare and how multiple providers will contribute to the overall payment.
Key Information to Include
Start by listing the personal and insurance information of the individual. This should include the individual’s full name, insurance policy number, and the names of the insurers involved. The document should also detail the services rendered and the costs associated with them. Be sure to include any relevant dates, such as the date of service and when the coverage decisions were made. The clearer the details, the easier it will be for the recipient to understand the content.
Formatting and Clarity
The layout of the communication should be simple and easy to read. Use bullet points or tables to organize financial information, so the recipient can quickly identify which expenses are covered and which are not. Keep language straightforward and avoid complex jargon to ensure that the message is clear to all parties. This will reduce confusion and help the recipient follow the necessary steps without hesitation.
Essential Elements in a Coordination Letter
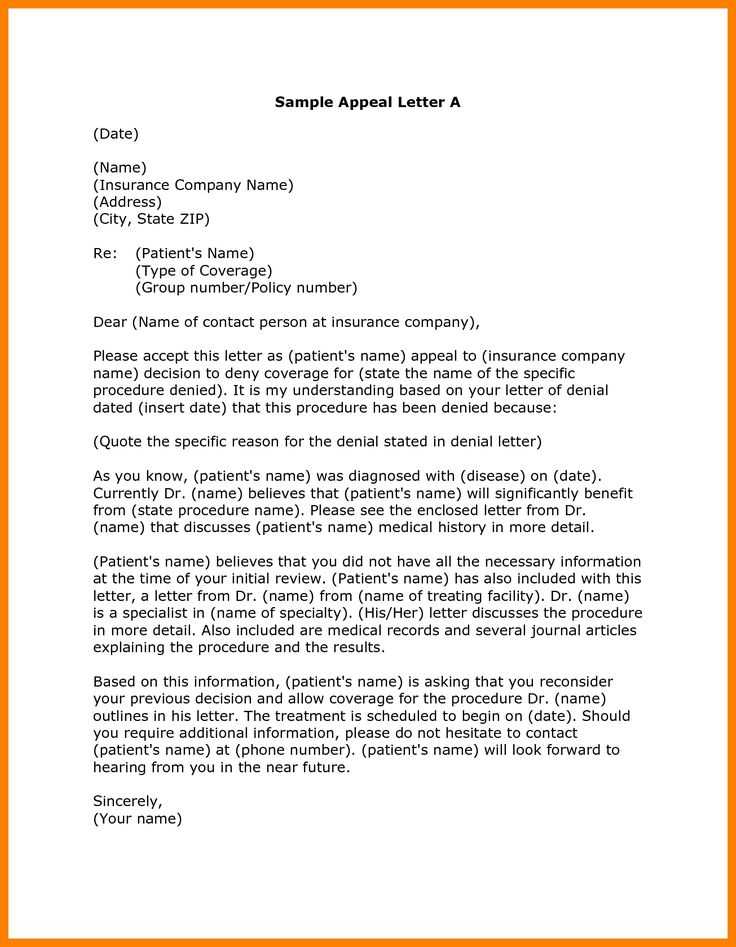
Creating a comprehensive and effective notification involves including several key components that ensure clarity and prevent confusion. These essential elements serve as the foundation for clear communication between insurers, healthcare providers, and individuals. Each piece of information must be structured in a way that is easy to understand and acts as a guide for the recipient.
- Personal Information: Include the individual’s full name, address, and insurance policy number for identification purposes.
- Insurance Details: List the insurers involved, including policy numbers and coverage details for each provider.
- Service Information: Clearly describe the healthcare services provided, including dates of service and the specific treatments received.
- Financial Breakdown: Provide a clear outline of costs, indicating which expenses are covered by each insurer and which remain the responsibility of the individual.
- Action Steps: Specify any required actions from the individual or the healthcare provider, such as submitting additional documents or following up with insurers.
By including these elements, the notification helps ensure that all parties are informed and understand their roles in the coverage process. A well-organized document minimizes confusion and ensures a smoother process for both the insured and the insurers involved.
Why Accurate Information Matters
Providing precise and complete details is essential when communicating with insurers and healthcare providers. Any inaccuracies in the documentation can lead to significant delays, miscommunication, and even the denial of claims. Ensuring that all information is correct and up-to-date helps avoid these issues and guarantees that the process runs smoothly for everyone involved.
Impact on Timeliness
Incorrect or incomplete data can cause delays in claim processing, which could affect an individual’s access to care or reimbursement. When insurers cannot verify the details provided, they may need to request additional information or make follow-up inquiries, slowing down the entire procedure. Accurate information expedites the resolution of any claim and ensures that services are covered as intended.
Avoiding Unnecessary Costs
Inaccuracies can also lead to financial complications. If details about coverage or payments are incorrect, it might result in unexpected out-of-pocket expenses for the individual. Providing the correct details in the document helps ensure that the right party is billed, preventing unnecessary financial burden on the insured.
Avoiding Common Template Errors
Errors in official documents can lead to confusion, delays, and complications in processing. It is crucial to ensure that all fields are filled out accurately, and the information is presented in a clear and consistent manner. By avoiding common mistakes, you can streamline the entire communication process and avoid unnecessary follow-up or rejection of claims.
- Incomplete Information: Leaving out essential details such as policy numbers, dates of service, or provider information can cause major issues. Always double-check that all required fields are fully completed.
- Incorrect Formatting: Using inconsistent formats for dates, amounts, or other key information can create confusion. Stick to standard formats for readability and ease of processing.
- Misspelled Names or Numbers: Small mistakes, such as misspelling an individual’s name or incorrectly entering an insurance number, can invalidate the entire document. Accuracy is key to ensuring proper identification and verification.
- Failure to Include Required Actions: If the recipient needs to take specific steps, ensure these instructions are clearly outlined. Neglecting to mention necessary actions can result in delays or missed opportunities.
By staying mindful of these common errors, you can ensure that all parties involved receive clear, accurate, and timely information, making the entire process more efficient and effective.