Otezla appeal letter template
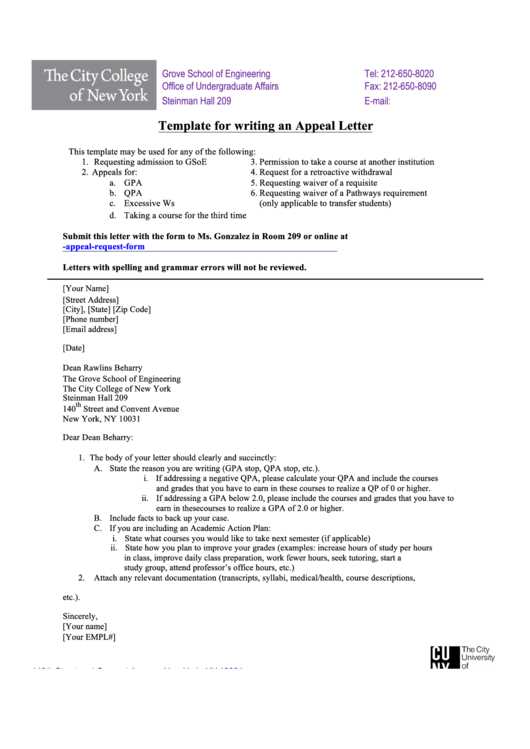
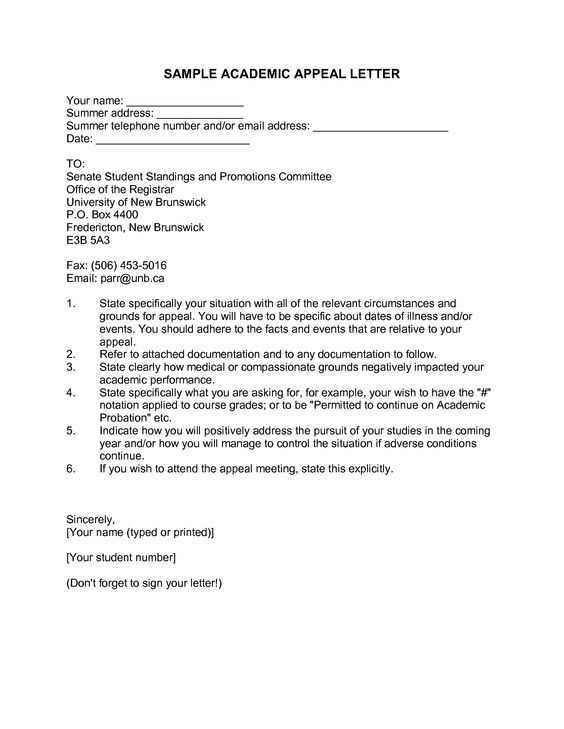
Structure Your Appeal Clearly
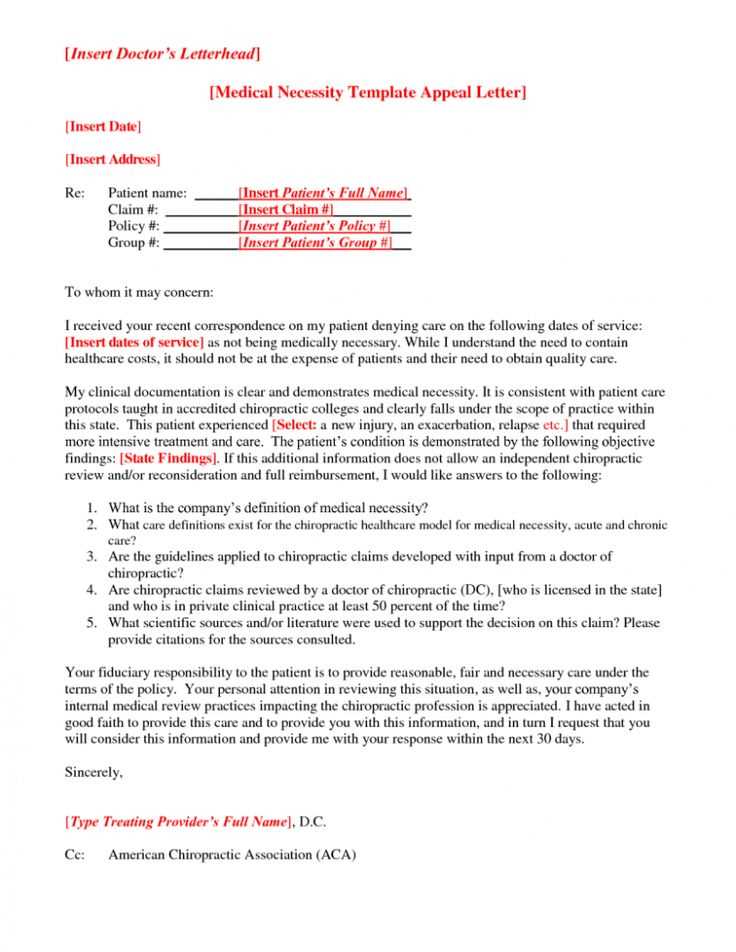
Focus on presenting your case in a well-organized way. Start by addressing the letter to the appropriate contact within the insurance company or provider. Include the details of the denial, such as the claim number and date of the decision. This helps establish the context right away.
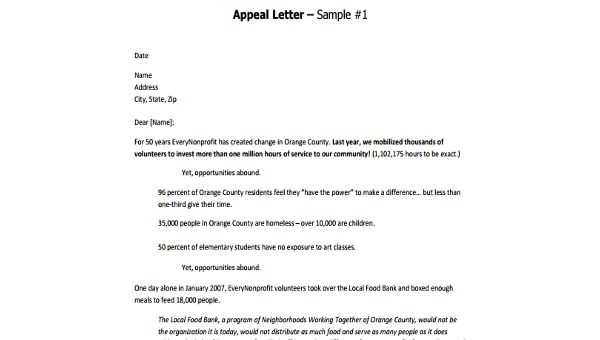
Introduce Your Situation
Begin with a clear statement of your condition and how Otezla has been an integral part of your treatment plan. Mention your healthcare provider’s recommendation for the medication, emphasizing how it has worked for you or how it is essential for managing your health condition.
Point Out the Denial Issue
Address the reason for the denial directly. If the denial was based on cost, alternative treatments, or insufficient evidence, highlight any mistakes or misunderstandings in the initial evaluation. If you have additional medical evidence or letters from your doctor, reference those as supporting documents.
Clarify Your Request
Clearly state that you are requesting a reconsideration of the denial. Specify that you are seeking approval for Otezla based on your medical need and the recommendation of your healthcare provider. Be concise but direct in explaining what you are asking for.
Support Your Appeal with Documentation
Attach relevant documents, such as medical records, a letter from your doctor, or any additional evidence that supports your case. Make sure to reference these documents in your letter to reinforce your points.
- Medical records detailing your condition
- Physician’s letter outlining the treatment plan
- Any previous treatment history that supports the need for Otezla
Conclude with a Positive Request
End the letter on a positive note, thanking the reader for their time and consideration. Express confidence that the appeal will be reviewed fairly, and state your readiness to provide further information if needed.
Tip: Always check for specific instructions on the appeal process from your insurance company or provider before submitting your letter. This ensures that you follow all necessary steps and avoid delays in processing.
Otezla Appeal Letter Template
To create a strong appeal letter for Otezla, start by addressing it directly to the insurance company or Medicare provider. Clearly state that you are requesting a reconsideration of a denial for Otezla coverage. Include your full name, policy number, and other identification details they may need to locate your file.
How to Structure Your Appeal Letter for Otezla
Begin with a concise introduction, stating your purpose–appealing the denial of coverage for Otezla. Follow this with a clear summary of the facts, including the date of the initial request, the reason for denial, and any medical details that may support your case. Provide your healthcare provider’s contact details and any relevant medical records.
Key Points to Include in the Request
Highlight why Otezla is the appropriate treatment for your condition. If applicable, refer to prior treatments and their lack of effectiveness. Include a detailed explanation of your medical history and the physician’s recommendation for Otezla as the next treatment option. Be sure to mention any trials or tests that show why this medication is necessary.
Common Mistakes to Avoid When Writing the Letter
Avoid being vague or overly emotional in your appeal. Stick to facts, and do not use generalized statements. Ensure all requested documents are attached, and double-check that your letter is free of typos or errors. Failing to include required medical documentation or not following up after submitting your appeal can delay the process or lead to a denial.
Understanding the Process for Otezla Coverage Appeal

After submitting your appeal, it will typically be reviewed by a panel of medical professionals or insurance representatives. They will evaluate your case based on medical necessity, previous treatments, and the supporting documentation you provide. The review process may take several weeks, and you may receive a final decision or be asked for additional information.
Important Documents to Attach with the Request
Attach your denial letter, medical records, a letter from your physician outlining the medical need for Otezla, and any other supporting documentation such as laboratory results or previous treatment records. If the insurance company requires a specific form, make sure to include that as well.
Steps to Follow After Submitting Your Appeal
Follow up within 2-4 weeks to check on the status of your appeal. If additional information is requested, respond promptly. If your appeal is denied again, you may have the option to escalate the process or file an external review, depending on your insurance policy or provider guidelines.