Letter of medical necessity for physical therapy template
Patient Information
Provide full name, date of birth, and relevant health insurance information for the patient requesting physical therapy. Include any known diagnoses or injuries that support the need for treatment.
Physician Information
Include the physician’s name, contact information, and professional credentials. Confirm that the physician is the primary care provider or specialist overseeing the patient’s care.
Medical Diagnosis
Describe the patient’s condition that necessitates physical therapy. Be specific about the diagnosis, noting any symptoms or limitations the patient is experiencing due to their condition.
Treatment Goals
Outline the goals for physical therapy. These should be based on the patient’s individual needs and treatment plan, such as improving mobility, reducing pain, or strengthening muscles.
Medical Justification
Explain why physical therapy is required for this patient. Support the necessity with specific details on how physical therapy will benefit the patient’s recovery and daily functioning.
Duration and Frequency
Provide a recommended timeline for treatment. Include how often the patient should attend sessions and the anticipated duration of the therapy plan.
Physician’s Signature
End the letter with the physician’s signature, confirming the medical necessity of physical therapy. Ensure the letter is dated and includes contact information for any follow-up.
Letter of Medical Necessity for Physical Therapy Template
Understanding the Purpose of the Letter
Key Components to Include in the Template
How to Customize the Letter for the Patient’s Needs
Formatting and Professional Language Advice
How to Address Insurance Criteria
Common Errors to Avoid When Writing
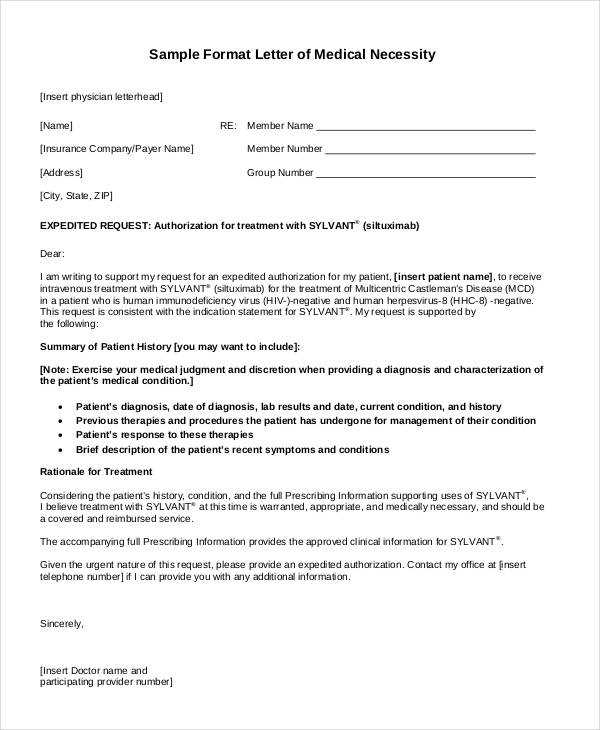
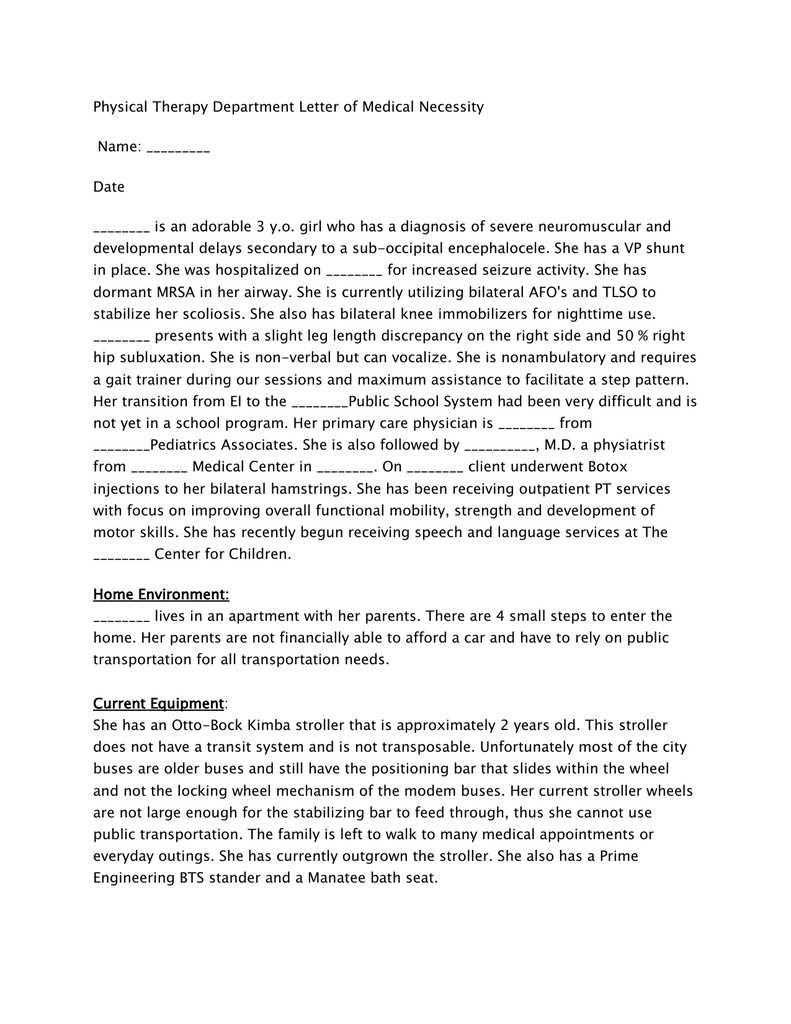
The letter of medical necessity serves as a formal request to insurance companies, providing the necessary justification for physical therapy services. It clearly outlines why the treatment is required and how it will benefit the patient’s health. Properly structured, it helps ensure the insurance provider understands the need for therapy and its long-term impact on recovery.
Key Components to Include in the Template
A complete letter should include specific information such as the patient’s diagnosis, treatment plan, goals, and expected outcomes. Begin with a concise explanation of the patient’s condition, followed by a detailed treatment plan tailored to address that condition. Outline how the therapy aligns with the patient’s recovery process and any previous treatments or interventions that were unsuccessful.
How to Customize the Letter for the Patient’s Needs
Personalize the letter by detailing the patient’s medical history and how physical therapy directly impacts their condition. Highlight any specific physical limitations or pain the patient is experiencing, and demonstrate how therapy will improve their functional abilities. Including relevant data such as test results or medical imaging can strengthen the case.
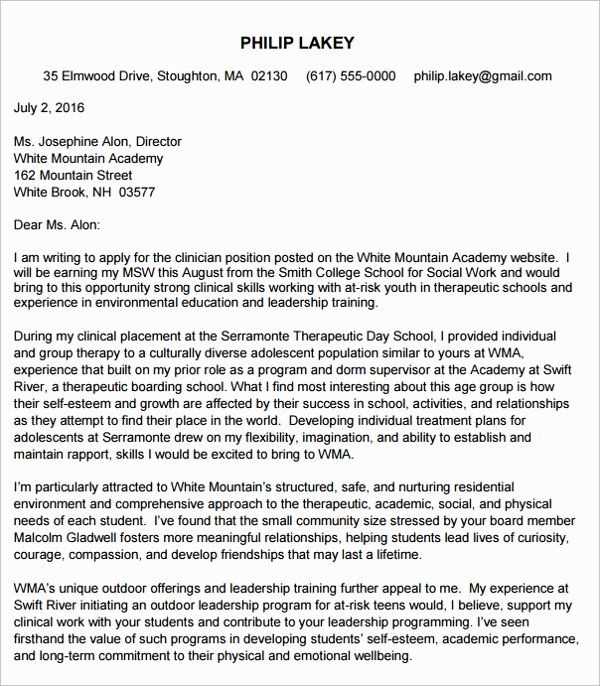
Formatting and Professional Language Advice
Maintain a formal and professional tone throughout the letter. Ensure clarity by organizing the content into well-defined sections, such as diagnosis, treatment plan, and expected outcomes. Use straightforward language and avoid jargon to make it easily understood by both medical professionals and insurance representatives.
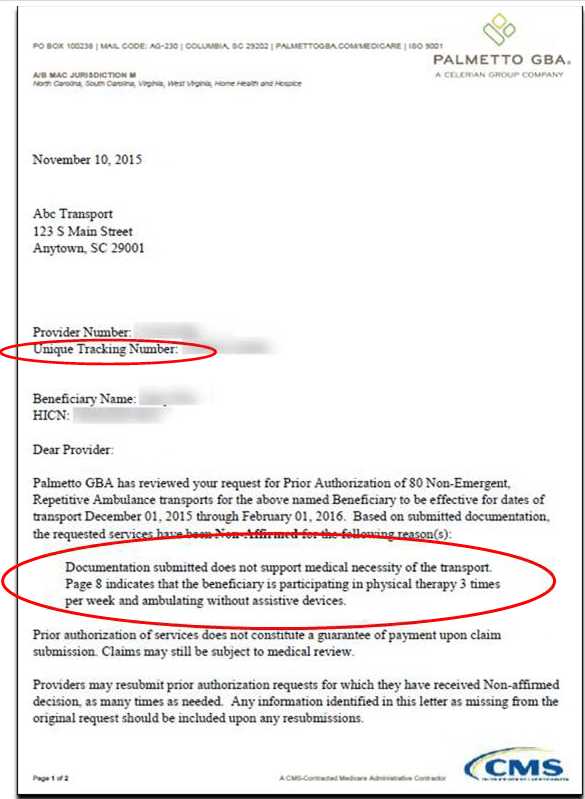
How to Address Insurance Criteria
Many insurance providers require proof that the treatment is medically necessary. Reference the insurance company’s specific criteria for physical therapy coverage and align the letter with those requirements. Provide clear explanations of how the treatment is linked to the patient’s diagnosis and why it is essential for recovery. Include any supporting documentation such as physician recommendations or prior authorization forms if necessary.
Common Errors to Avoid When Writing
Avoid vague statements or generalizations that do not provide specific evidence of necessity. Ensure all information is accurate and up-to-date, as inaccuracies can lead to delays in approval. Double-check the patient’s information and make sure all medical terms are used correctly. Additionally, avoid overly technical language that might confuse insurance reviewers or hinder the clarity of the request.